Abortion and Criminal Justice Bill
Selaine’s response:
I completely understand what an incredibly emotive issue abortion is, and I appreciate the strength of feelings on both sides. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion and allows Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
I have noted all views on the amendments proposed to the Criminal Justice Bill. These amendments, and all other provisions made in this Bill, will be discussed as it progresses through both Houses. It is essential, as with all pieces of legislation, that this Bill is subject to proper debate and formal parliamentary scrutiny.
At this time I have not added my name to Sir Liam Fox's Down Syndrome abortion amendment, as I believe like all the abortion amendments that we should not be discussing such amendments in this Bill. I do understand the importance of this amendment, and should the matter be voted on, I have assured Sir Liam Fox of my support.
I know that making a decision regarding abortion can be extremely difficult, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all their options, with medical professionals offering impartial advice. I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion including all options available to them.
May 2024
Scope: An Equal Future
Selaine’s response:
To alleviate some of the pressures that disabled people are facing with the cost of living, the Government is providing extensive support to disabled people and those with long term health conditions. The Government is committed to ensuring disability is not an obstacle to living a full, independent life where people can reach their full potential.
In recognition of the exceptional circumstances of the last two years, the Government has taken decisive action to provide timely relief to those with disabilities and health conditions. On 6 April 2024, disability benefits, including Personal Independence Payment, Disability Living Allowance, and Employment and Support Allowance, were increased by 6.7 per cent. In 2023/24, the Government will spend around £78.6bn on benefits to support disabled people and people with health conditions.
Last year, more than 6.4 million individuals received a £150 Disability Cost of Living Payment. This was in addition to three payments totalling £900 for those on means tested benefits, and the extension of the Household Support Fund, which has provided 26 million awards for vulnerable families.
Regarding employment, between Q1 2017 and Q1 2022, the number of disabled people in the UK in employment increased by 1.3 million. This means that the goal to see a million more disabled people in employment between 2017 and 2027 has been met and exceeded five years ahead of schedule.
There is, however, more to do, particularly in reducing the disability employment gap even further. The Back to Work Plan sets out steps to support those with disabilities and long term health conditions to enter into employment, while the National Disability Strategy and Disability Action Plan are working to improve the daily experiences of disabled people, ensuring this country is the most accessible and equal place to live in the world.
The Work and Pensions Select Committee which I have been a part of since my election is currently holding an inquiry into progress made in supporting disability employment, and I am following the evidence closely.
May 2024
Assisted Dying Petition Debate
Selaine’s response:
Coping with terminal illness is distressing and difficult both for the patient and their families. These cases are truly moving and evoke the highest degree of compassion and emotion.
As a general principle, I believe individuals should have as much control as possible over their own lives, therefore I am broadly supportive of a change in the law to allow assisted dying for the terminally ill and mentally competent.
However, we must be careful to ensure changes in the law do not encourage anybody to make the decision to end their life. New or amended legislation should only allow those who are already determined to end their lives to do so without their loved ones having to endure difficult legal processes afterwards.
I also completely understand why others feel equally strongly against assisted dying, and their views must be respected. I feel it is right that this issue falls under an ‘issue of conscience’ in Parliament, so that MPs can vote in accordance with their own beliefs, free from political constraints.
In the case of me voting on the matter, I would take into account the stories I have heard from constituents, who too feel strongly about this emotive issue. However, as it stands, ministerial colleagues have made clear that the Government is not planning to bring forward legislation on assisted dying in spite of recent comments from Dame Esther Rantzen. The Health and Social Care committee’s inquiry into these matters is independent of Government, which takes a neutral stance. This means changes would need to be implemented via a Private Members’ Bill. In the instance it became the clearly expressed will of Parliament to amend or change the criminal law so as to enable some form of assisted dying, the Government would undertake the role of ensuring such relevant legislation was delivered as effectively as possible.
While I thank my constituents for inviting me to attend the Westminster Hall debate on April 29, I am unfortunately unable to attend but will continue to listen to a range of views on this highly sensitive matter.
April 2024
Pancreatic Cancer
Selaine’s response:
Given that the UK ranks 15th out of 16 European countries for five year pancreatic cancer survival, more must be done to increase early diagnosis to reduce the survival gap between pancreatic cancer and other cancers. The NHS Long Term Plan set an ambition to improve these outcomes, so that 75 per cent of all cancers can be diagnosed at stage 1 and 2 by 2028 when it is easier to treat.
This ambition will be achieved through ongoing work between the Department of Health and Social Care to increase early diagnosis and survival rates for pancreatic cancer. Through the Elective Recovery Plan, the Government is investing £2.3 billion to create more Community Diagnostic Centres which will be prioritised for cancer services.
A Faster Diagnosis Standard for cancer will be introduced so that patients who are referred urgently or identified by NHS cancer screening have a maximum 28 day wait for being told definitively whether they have cancer. In addition, there will be a maximum 31 day wait from a decision to start any cancer treatment for all cancer patients.
My understanding is that the NHS is also implementing non specific symptom (NSS) pathways for patients who present with vague and non site specific symptoms (including pancreatic cancer symptoms) which do not align clearly to a tumour type. The NSS programme aims to achieve full population coverage across England for NSS pathways by March 2024.
I will continue to support Pancreatic Cancer UK and the Union for International Cancer Control, both of which raise awareness of cancers requiring early diagnosis and treatment. I attended World Cancer Day’s Less Survivable Cancers Taskforce drop in last year to show support for closing the #DeadlyCancerGap, and this January attended Pancreatic Cancer UK’s Parliament drop in to support the Don’t Write Me Off Campaign, and awareness for the Optimal Care Pathway proposal.
April 2024
Health and Equality Acts (Amendment) Bill
Selaine’s response:
The Private Members’ Bill, which seeks to address specific issues in relation to transgender or gender questioning children and to redefine the meaning of “sex” in the Equality Act 2010, was scheduled to have its second reading on Friday 15 March.
MPs did not have the opportunity to debate this Bill on its scheduled date due to filibustering by the Labour Party, which I witnessed first hand as my own Private Member’s Bill was on the same day. However, more broadly, the Government welcomes the sentiment set out in the Bill, and is clear that biological sex exists and matters, and is committed to maintaining the safeguards that allow organisations to provide single sex services. The Government has already begun addressing these complex issues in a pragmatic and proportionate way and will continue to do so.
In October 2023, the Government announced that it will change the NHS Constitution to clarify patients’ rights to access separate and single-sex spaces in hospitals and address patient concerns about patient choice on intimate and personal care, ensuring that women have the right to access dedicated single sex spaces.
The Government has welcomed the decision by NHS England to no longer routinely prescribe puberty blockers at gender identity clinics, which will help ensure that care is based on evidence, expert clinical opinion and is in the best interest of patients. I understand that it is expected the private sector will follow suit, and if a private organisation registered with the Care Quality Commission fails to meet the conditions of its registration, then the regulator can take enforcement action.
Additionally, the Department for Education and Minister for Women and Equalities, have introduced guidance, which was developed alongside experts, to support schools both in relation to transgender pupils and those who are questioning their gender. This guidance is categorical that social transition is not a neutral act, and that social transition, in practice, should be extremely rare when the appropriate safeguards are put in place and the child’s best interest taken into account. You will be reassured to know that safeguarding should always remain a priority for schools, and that they have a legal duty to protect single-sex toilet spaces and maintain safety in single sex sports.
The Government does recognise that more can be done in this area, which is why the Minister for Women and Equalities has commissioned detailed policy and legal analysis into the meaning of sex in the Equality Act, which is underway.
March 2024
NHS Waste
Selaine’s response:
Existing NHS England guidelines advise NHS Trusts to reuse medical equipment when safe and appropriate to do so. For example, trusts are encouraged to reuse crutches, frames and walking sticks to help improve access for patients and save money. This also provides an excellent opportunity for carbon savings due to the high greenhouse gas intensity of aluminium manufacture.
Trusts are also encouraged to set up dedicated walking aid return and reuse schemes. This will ensure that walking aids are only returned to a designated walking aid drop off location where they can then be assessed using a simple procedure of checks, parts replacement, and cleaning to ensure they are safe for reuse.
Furthermore, the Medical Technology Strategy, published in February 2023, committed to developing an environment to deliver value for money and affordability across the whole patient pathway for medical supplies and equipment. As part of this commitment, the Department is working closely with NHS England and NHS Supply Chain alongside industry and patient groups to develop a consistent methodology for assessing value in terms of outcomes and not just unit cost, which will be adopted at both a national and local level.
February 2024
Conversion Therapy
Selaine’s response:
I know that legislation to ban so called 'conversion therapy' was not announced in the recent King's Speech.
I can assure constituents that a lot of work has already been done, particularly with faith groups to enable ideas and solutions to be brought forward. I understand that ministers are still reviewing this and continue to be committed to tackling conversion practices, and are very aware that the public want a decision. The Government is taking great care to protect people who might be vulnerable to these kinds of practices.
January 2024
Patient Safety
Selaine’s response:
Patient safety is central to our NHS, ensuring that people are able to seek the care that they need with the confidence they will be safe doing so.
The Government has established the Health Services Safety Investigations Body as an independent statutory body, through the Health and Care Act. This builds on the work of the Healthcare Safety Investigations Branch, with the function of investigating incidents that occur in England during the provision of health care services which have, or may have, implications for the safety of patients. I fully support these steps to empower staff and patients to report incidents, enabling NHS staff to learn and better protect future patients.
In December 2021, the Government published its response to the findings of the inquiry into the issues raised by disgraced surgeon, Ian Paterson. The Government accepted the overwhelming majority of the recommendations made by the inquiry and set out an implementation plan of 40 actions to put those recommendations into effect. The Government published a progress report on the implementation plan in December 2022. The report provides full details of this progress against the four themes of the Government’s response as laid out in the implementation plan, and demonstrates that good progress has been made.
In 2021, the Government responded to the Independent Medicines and Medical Devices review and set out an ambitious programme of change centred on patient safety. The main features are improving how the system listens to and responds to concerns raised by patients, strengthening the evidence base on which decisions are made, and improving the safety of medicines and devices.
I was encouraged to see the outcome of the consultation on the role of a Patient Safety Commissioner, acting on the second recommendation of the Review. Views were sought on a range of proposals from terms of office to remuneration and, in light of support for each proposal, the Government will proceed with them. I welcome the appointment of Dr Henrietta Hughes OBE as the first ever Patient Safety Commissioner for England in July 2022.
Further, the NHS published a Patient Safety Strategy in 2019 and this is updated yearly. This plan sets out how the NHS looks to continuously improve patient safety, building on the foundations of a safer culture and safer systems.
January 2024
Dementia Diagnosis and Research
Selaine’s response:
There are currently 900,000 people living with dementia in the UK and this is projected to rise to 1.6 million by 2040, so research is crucial to understanding the condition and improving outcomes for those affected. I visited Dementia UK at the North Devon District Hospital, I found the visit very insightful and moving.
Unfortunately, I was unable to attend the Westminster Hall debate on new dementia treatments. The Government is committed to supporting research into dementia and has committed to double funding for dementia research, to £160 million per year by 2024/25.
In August 2022, the Dame Barbara Windsor Dementia Mission was launched along with £95 million of Government funding. The Mission is part of the commitment to double dementia research funding and aim to speed up the development of new treatments.
A new taskforce, made up of industry, the NHS, academia and families affected by dementia, will lead this work to allocate dementia funding. You can register your interest to take part through the Join Dementia Research website here: https://www.joindementiaresearch.nihr.ac.uk/
The National Institute for Health and Care Research has also launched a number of new initiatives to support dementia research, such as investing nearly £11 million to develop new digital approaches for the early detection and diagnosis of dementia.
Finally, the Government has announced its intention to develop and publish a Major Conditions Strategy. The strategy will set out a strong and coherent policy agenda that sets out a shift to integrated, whole person care. Interventions set out in the strategy will aim to alleviate pressure on the health system, as well as support the Government’s objective to increase healthy life expectancy and reduce ill health related labour market inactivity. Dementia is one of the six major conditions included in the strategy.
Last year, the Government held a call for evidence for the Major Conditions Strategy. The Government is analysing evidence received and will respond in due course.
January 2024
At Home Early Medical Abortion (Review) Bill
Selaine’s response:
Please note that I do not sign any Early Day Motions (EDMs). These have no chance of becoming law, and according to the House of Commons Library, cost £271 each to publish. I do not feel that this is a good use of taxpayer’s money, nor do I feel that this is an effective way to raise an issue in Parliament.
Safeguarding is an essential aspect of abortion care, and the Department’s Required Standard Operating Procedures (RSOPs) for approved independent sector abortion providers in England include the requirement that all abortion providers have effective arrangements in place to safeguard vulnerable women accessing home-use early medical abortion who may be experiencing coercion to end a pregnancy. Providers must ensure that all staff are trained in recognising the signs of potential abuse and coercion and know how to respond.
The Care Quality Commission (CQC) inspects against all the Department’s RSOPs when it inspects an independent sector provider, and safeguarding procedures are included in the CQC’s Termination of Pregnancy inspection framework as areas to be considered during an inspection.
As commissioners of abortion care, NHS England and integrated care boards are responsible for ensuring abortion providers have appropriately trained staff to meet safeguarding requirements.
The standard of training for healthcare professionals is the responsibility of the health care independent statutory regulatory bodies who set the outcome standards expected at undergraduate level and approve courses. Higher Education institutions write and teach the curricula content that enables their students to meet the regulators outcome standards. Whilst not all curricula may necessarily highlight a specific condition, they all emphasise the skills and approaches a health care practitioner must develop to ensure accurate and timely diagnoses and treatment plans for their patients, including for abortion.
I would like to stress that home use of early medical abortion pills is only permitted if the pregnancy has not exceeded 10 weeks gestation at the time the first medicine in the course is administered. If there is any uncertainty about the gestation of the pregnancy, the woman should attend an in person appointment.
January 2024
Anaesthesia and Physician Associates
Selaine’s response:
I note the concerns about the training and competency of anaesthesia and physician associates, but disagree with your assessment of the roles. As you may be aware, the physician associate (PA) title has been well established in the United Kingdom since 2014.
It is also important to note that during training and qualified practice PAs must work with a dedicated medical supervisor which will be a consultant, GP, or other senior medical personnel.
This medical supervisor is responsible for the supervision and management of a student’s educational progress throughout the clinical placements of the course. However, practicing PAs, nurses and other healthcare professionals can train, supervise, and assess a PA student in a particular skill, procedure, or competence.
At present, the Faculty of Physician Associates at the Royal College of Physicians also provides professional support to PAs across the United Kingdom. The Faculty’s support includes setting standards for education and training, as well as overseeing a voluntary register of qualified PAs who have been declared fit to practise in the UK.
The Government laid legislation before Parliament on Wednesday 13 January 2024 to begin the process of regulating PAs and AAs, which will allow the GMC to commence regulation by the end of 2024. Regulation by the GMC will help provide clear standards for the clinical practice and professional conduct of PAs and make it easier for employers, patients, and the public to understand the relationship between this role and that of doctors.
NHS England is working with the relevant professional colleges and regulators, to ensure the PA and AA roles are expanded safely and effectively. The new regulation will help ensure that PAs and AAs have the same levels of regulatory oversight and accountability as doctors and other regulated healthcare professionals.
January 2024
Nursing
Selaine’s response:
I would like to start by saying that I am extremely grateful for the dedication of nursing staff in very difficult circumstances over the last three years and a special thanks goes to the nurses at North Devon District Hospital for all their hard work. I appreciate that the challenge of working in the NHS during the pandemic, and through the current period when the demand for patient care is very high, has taken a significant toll on nurses.
The last few years have also amplified existing challenges in the nursing workforce, such as the ability to retain experienced nursing staff to continue working in the NHS. Extending flexible working is one way to alleviate these challenges in several professions, so that NHS staff have greater choice over their working patterns and achieve a better work life balance.
Throughout, the Government’s approach has been to protect the safety of both patients and staff. As a result of talks between the Government, NHS employers and the unions, an offer was made for NHS staff (including nurses) to receive an additional pay rise of 2 per cent for 2022-23, on top of the 4% increase awarded by the Government through the Independent Pay Review Body process.
A "Backlog Bonus" of at least £1,250 will also be paid in recognition of the dedication and efforts of NHS staff during the pandemic and their role in cutting waiting lists. The level of bonus will be determined by pay band and experience, so for example, the average nurse in pay band 5, will receive £1,350.
For 2023-24, the Government offered NHS staff a 5% consolidated increase in pay, worth at least £1,065. Alongside this, the Government will introduce measures to ensure safer staffing in hospitals, make the pension abatement rules introduced during the pandemic permanent and identify ways to tackle violence against NHS staff.
The Government has also provided a commitment to the RCN to address specific challenges around recruitment, retention and professional development in nursing, and will also consider a separate pay spine exclusively for nursing staff in 2024-25.
I firmly believe that this agreement represents a fair and reasonable offer for NHS staff, as well as being a fair deal for taxpayers. The NHS Staff Council, which includes unions and NHS employers, voted to accept this pay deal. The Government ensured that the deal was implemented so that more than a million workers across the NHS (including nurses) could receive this extra pay from June 2023.
January 2024
Dementia Diagnosis and Research
Selaine’s response:
An estimated one million people will be living with dementia by 2025, so research is crucial to understanding the condition and improving outcomes for those affected. I was proud to stand on a manifesto that committed to doubling dementia research funding and finding a cure for dementia.
In memory of the late Dame Barbara Windsor, the Government launched a new mission in 2022 to put this into practice. Research funding for dementia will rise to a total of £160 million a year by 2024, with an additional £95 million being provided to increase clinical trials and research projects.
A new taskforce, made up of industry, the NHS, academia and families affected by dementia, will lead this work to allocate funding. You can register your interest to take part through the Join Dementia Research website here: https://www.joindementiaresearch.nihr.ac.uk/
Finally, the Government has announced its intention to develop and publish a Major Conditions Strategy. The strategy will set out a strong and coherent policy agenda that sets out a shift to integrated, whole person care. Interventions set out in the strategy will aim to alleviate pressure on the health system, as well as support the Government’s objective to increase healthy life expectancy and reduce ill-health related labour market inactivity. Dementia is one of the six major conditions included in the strategy.
On 17 May, the Government launched its call for evidence for the Major Conditions Strategy which ran until 27 June. The Government is analysing responses and will respond in due course.
November 2023
Mental Health Bill
Selaine’s response:
I firmly support the Government's commitment to see mental health treated on a par with physical health, and I supported proposals to reform the Mental Health Act 1983 (MHA). I understand that the Government is reviewing the outcome of the Joint Committee on the Draft Mental Health Bill's pre legislative scrutiny report and will respond in due course.
I recognise that there is disappointment that a Bill was not included in the recent King’s Speech. However, I understand that the Government remains committed to bringing forward a Mental Health Bill when Parliamentary time permits.
In the meantime, the Government will continue to take forward non legislative commitments to improve the care and treatment of people detained under the Act. Ministers' intention to achieve parity of esteem is also reflected in the historic levels of investment the Government is putting into NHS mental health services. The £2.3 billion of additional funding per year by March 2024 will expand and transform mental health services, enabling two million additional people to benefit from mental health support.
The Government has also recognised the need to improve the mental health estate. The NHS is on track with a commitment to eradicate dormitories in mental health inpatient care by next year, replacing them with single patient rooms which improve dignity and outcomes for patients. Progress is underway to improve care for people undergoing a mental health crisis, with £150 million capital investment in 50 schemes including crisis cafes, crisis houses, and new and improved health based places of safety which provide a safe space for people detained by the police.
The Government also continues to pilot models of Culturally Appropriate Advocacy, providing tailored support to hundreds of people from ethnic minorities to improve understanding of their rights when they are detained under the MHA. Earlier in 2023, the Department of Health and Social Care also published a suicide prevention strategy, with an ambitious commitment to see the suicide rate fall within two and half years.
November 2023
Carers and Unpaid Carers
Selaine’s response:
I recognise the valuable contribution made by carers of all kinds, residential, domiciliary, paid, unpaid, many of whom spend a significant proportion of their life providing support to family members, friends and neighbours.
I note the concerns raised by the Carer Poverty Coalition. All future funding commitments are a matter for the Treasury, which has outlined its spending plans in the Autumn Statement.
I completely agree that carers must receive the right support to help them carry out their caring roles. A tenth of adults in the UK provide unpaid care for a friend or family member, and these people should be supported in the invaluable work they do.
The Government is continuing to support the implementation of improved rights for carers, enshrined in the Care Act 2014. Carers can receive support through the Carer Element in Universal Credit and through Pension Credit and Carer's Allowance has been increased to £69.70 per week. Over the last twelve years successive changes will have provided an additional £800 a year for carers.
The Government’s Social Care White Paper outlined a number of measures to support carers including up to £25 million to kick start a change in the services provided to support unpaid carers. The Carer’s Leave Act has also been introduced to give unpaid carers the right to take unpaid leave from work to care for older, disabled or seriously ill relatives.
Local authorities are also required to undertake a Carer's Assessment for carers who require support. This may include recording a career's needs and the impact of providing care. Local authorities have a legal duty to meet a carer's needs if these are assessed as being eligible for support.
Going forward, NHS England at a national level and Integrated Care Boards at a local level will have a duty to involve carers when care is being commissioned for their loved one. The Department for Education will be amending the School Census to include young carers. In 2023/24, £327 million of Better Care Fund funding has been earmarked to provide short breaks and respite services for carers, as well as additional advice and support.
The Government understands that people are worried about the cost-of-living challenges ahead and has announced further support for the next financial year designed to target the most vulnerable households. This cost of living support is worth £26 billion in 2023/24, in addition to benefits uprating, which is worth £11 billion to working age households and people with disabilities. This support for 2023/24, is on top of the £37 billion of support for the cost of living already in place to support households in 2022/23, in addition to the Energy Price Guarantee.
November 2023
Suicide Prevention
Selaine’s response:
I note the campaign being run by Samaritans about local funding for suicide prevention. All future funding commitments are a matter for the Treasury, which has outlined its spending plans in the Autumn Statement. However, I hope that the Government’s delivery of record investment in mental health services (£15.9 billion just in this financial year which is 28%more funding than in 2018) should give confidence that this Government is committed to improving mental health services.
November 2023
Coerced Abortion
Selaine’s response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings on both sides. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion and allows Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
Unfortunately, I was unable to attend the parliamentary event being hosted by the Society for the Protection of Unborn Children due to prior commitments.
The approach to abortion in Great Britain is set out in the Abortion Act 1967, which states that two doctors must certify that, in their opinion, a request for an abortion meets at least one and the same ground laid out in the Act. These grounds include “risk to the life of the pregnant woman”, and “substantial risk that if the child were born it would suffer from such physical or mental abnormalities as to be seriously handicapped”.
Guidance for doctors on how to comply with the Act has been issued, which stipulates that registered medical practitioners should be able to show how they have considered the particular facts and circumstances of a case when forming their opinion. Full details can be found online at: www.gov.uk/government/publications/guidance-for-doctors-on-compliance-with-the-abortion-act.
I am aware that all independent sector abortion clinics in England have been reapproved, which will ensure that abortion services continue to be available to women across the country. I understand that all current approvals are valid until 31 July 2026.
I know that making a decision regarding abortion can be extremely difficult, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all their options, with medical professionals offering impartial advice. I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion including all options available to them.
November 2023
Pancreatic Cancer
Selaine’s response:
Given that the UK ranks 15th out of 16 European countries for five-year pancreatic cancer survival, more must be done to increase early diagnosis to reduce the survival gap between pancreatic cancer and other cancers. The NHS Long Term Plan set an ambition to improve these outcomes, so that 75 per cent of all cancers can be diagnosed at stage 1 and 2 by 2028 when it is easier to treat.
This ambition will be achieved through ongoing work between the Department of Health and Social Care to increase early diagnosis and survival rates for pancreatic cancer. Through the Elective Recovery Plan, the Government is investing £2.3 billion to create more Community Diagnostic Centres which will be prioritised for cancer services.
A Faster Diagnosis Standard for cancer will be introduced so that patients who are referred urgently or identified by NHS cancer screening have a maximum 28-day wait for being told definitely whether they have cancer or not. In addition, there will be a maximum 31-day wait from a decision to treat to any cancer treatment starting for all cancer patients.
My understanding is that the NHS is also implementing non-specific symptom (NSS) pathways for patients who present with vague and non-site specific symptoms (including pancreatic cancer symptoms) which do not align clearly to a tumour type. The NSS programme aims to achieve full population coverage across England for NSS pathways by March 2024.
November 2023
Pulmonary Hypertension
Selaine’s response:
I am unable to attend Action for Pulmonary Fibrosis’ event due to prior commitments. However, please be assured I will continue to follow this matter closely.
I know that correctly diagnosing PH or PF can sometimes take time because its symptoms, like shortness of breath, tiredness, chest pain and swelling in the legs, are similar to those of many other heart and lung conditions. I agree that it is vital to raise awareness of pulmonary hypertension to ensure that patients are able to recognise symptoms and manage their conditions.
The NHS Long Term Plan makes a number of commitments relating to respiratory and pulmonary diseases, including increasing the number of people receiving physical health checks by 110,000 people per year, which will in turn assist with earlier diagnosis of conditions like pulmonary hypertension.
Enabling more people with heart and lung disease to complete a programme of education and exercise based rehabilitation will result in improved exercise capacity and quality of life in up to 90 per cent of patients.
The most recent audit of services across all eight specialist PH centres in England and Scotland has shown that 11 of the 15 standards are being met nationally. However, there is always more that can be done to improve patient experience. Raising awareness of conditions such as pulmonary hypertension is a vital part of ensuring patients receive the support they need.
October 2023
Baby Loss
Selaine’s response:
This issue unfortunately affects many people, and I offer my sympathy to those who have suffered miscarriages, stillbirths, or the loss of a child. I applaud my colleagues who have recounted this painful experience in their lives in Parliament to raise awareness of baby loss and inspire changes in policy.
The UK is one of the safest places in the world to give birth. However, I know that the Government recognises that there is still more to be done. The Department of Health and Social Care has set out a range of measures to deliver its ambition to halve the rates of stillbirths, neonatal deaths and brain injuries that occur during or soon after labour, and maternal deaths by 2025 relative to levels in 2010.
I welcomed the publication of the Women's Health Strategy in July 2022 that made several commitments related to baby loss and maternity care. This included a pledge to introduce a pregnancy loss certificate in England as recommended by the interim update of the independent Pregnancy Loss Review. The Government has announced that a new Certificate of Pregnancy Loss will be available for bereaved parents to apply for from October this year.
The Government is focused on ensuring that bereaved parents feel able to navigate the complexities of the healthcare system and will put an emphasis on supporting them through their grief, recognising their loss, acknowledging their pain and ensuring they feel heard.
October 2023
Carer's Allowance
Selaine’s response:
Both the Government and I recognise and appreciate the vital role played by unpaid carers, and I understand that this is an extremely important issue for many carers.
The primary purpose of Carer's Allowance is to provide a measure of financial support for people who give up the opportunity of full time employment in order to care for a severely disabled person. It must be stressed that it is not a carer’s wage or payment for the services of caring, nor is it intended to replace lost or forgone earnings in their entirety.
The Carer's Allowance earnings limit is not linked to the number of hours worked. Instead, it is set at a level that aims to encourage people to maintain a link with the labour market through part time work. The earnings limit for Carer's Allowance is a net figure, meaning it takes into account Income Tax, National Insurance contributions, and half of any contributions to an occupational or personal pension, and there are also a number of other deductions which can be made. That means that people can earn significantly more than £139 per week gross and still be eligible for Carer's Allowance.
In April 2023, Carer's Allowance was increased by 10.1%, in line with inflation, from £69.70 to £76.75 per week.
I would encourage carers to check their eligibility for additional support, such as Universal Credit. Universal Credit can include an additional amount for carers who provide care of 35 hours or more each week for a severely disabled person. For carers who satisfy the qualifying criteria, an additional amount of £185.86 per month is included in their Universal Credit entitlement. For those receiving Universal Credit, the 55% taper rate and any applicable work allowance will help to ensure that people are better off in work.
October 2023
Vaping and E-Cigarettes
Selaine’s response:
While e-cigarettes are not risk free, the Government is actively supportive of the use of e-cigarettes as a means to help people stop smoking and contribute towards the goal of a smoke free England by 2030.
Some of the highest success rates of those trying to stop smoking are among people using an e-cigarette, with evidence suggesting that an additional 70,000 people stop smoking every year as a result of using these devices. An estimated 2.4 million vapers are former smokers, and Vaping Awareness Month, VApril, provides an opportunity to highlight the potential health benefits of making the switch.
I fully understand concerns by parents about underage sales of vapes, and the Government is actively taking steps to tackle this issue. A call for evidence ran over the summer to identify opportunities to reduce the number of children accessing and using vapes, and consider the environmental impact of disposable vapes. The next steps due will be announced in due course.
In the meantime, a new “illicit vapes enforcement squad”, led by Trading Standards and backed by £3 million of Government funding, has been set up to enforce the rules on vaping and tackle illicit vapes and underage sales. The enforcement squad will undertake specific projects like test purchasing in convenience stores and vape shops, and it will have the power to remove illegal products from shops and at our borders.
There is insufficient evidence to justify the prohibition of e-cigarettes, with the risk to the health of bystanders from e-cigarette vapour being low. In addition, there is no evidence of comparable harm from exposure to e-cigarettes compared to tobacco, so they are not covered by the legislation banning smoking in enclosed public spaces.
I am aware of media reports speculating about proposals that may come forward around the sale of disposable vapes. Over the last few months, the Department of Health and Social Care has been running a consultation to identify opportunities to reduce the number of children accessing and using vaping products, and explore where the Government can go further. Following the consultation, the next steps will be announced in due course.
I will continue to monitor this issue closely and look forward to reading any future proposals in relation to the use of vaping products.
October 2023
VPAS Campaign
Selaine’s response:
I note the concerns about the accessibility and affordability of medicines through the NHS and the findings of the report prepared by Global Justice, STOPAIDS and Just Treatment. However, having reviewed the report, I understand the Department of Health and Social Care does not recognise the methodology used to form its conclusions.
The voluntary scheme plays an important role in supporting sustainable patient access to the most clinically and cost effective medicines. The current voluntary scheme has enabled the NHS to deliver a record number of access deals for medicines. When VPAS expires at the end of 2023, it is expected to have generated around £7 billion of income for the NHS over nearly five years. At present, 90 per cent of companies supplying eligible health service medicines to the NHS are members of the voluntary scheme.
There are several other ways in which the Government improves the affordability of medicines for the taxpayer.
The Government has a statutory scheme for branded medicine pricing is in place for companies that do not opt into VPAS. A consultation on the future of the statutory scheme was published on 19 July 2023.
My understanding is also that companies must also agree a public “list price” for branded medicines with the Department before they can market it in the UK.
Furthermore, the National Institute for Health and Care Excellence also assesses the cost effectiveness of medicines before they are delivered through the NHS.
Negotiations between the Government and the pharmaceutical industry over a replacement to the voluntary scheme are ongoing, and are likely to conclude this autumn, with a potential new scheme coming into force in 2024. I am confident that this deal will strike the right balance between supporting access to medicines, whilst controlling costs and ensuring value for money for spending on medicines.
September 2023
National Care Service
Selaine’s response:
During this Parliament, the Government has made several proposals for reforming adult social care in England, including measures that would have provided additional funding, the Social Care White Paper and the social care cap. The Opposition has consistently opposed each of these proposals to date.
I am opposed to proposals for a National Care Service, and there are significant flaws in the Fabian Society's report (conducted on behalf of the Opposition) advocating for this approach. For example, the Fabian Society states that “delivering on people’s aspirations for what an NCS would achieve will require a very substantial increase in public funding over many years.” However, the report does not state the cost of such measures or how they would be paid for.
Current proposals for a National Care Service risk causing a complex, centralising, top-down reorganisation of health and social care across England. The Fabian Society’s report proposes new legislation that would impose new duties on central and local government, as well as introducing a national care guarantee, codified in a new National Care Service ‘constitution’. No information is provided on how the income would be raised to fund central and local government for the costs of these new duties, but the independent Kings Fund has stated that this would require wider reform of local government finance.
I also note that Labour MSPs have opposed similar proposals introduced by the Scottish Government, with criticism levelled at the top down centralisation, structural change and lack of clarity around what a National Care Service would cost to deliver.
In the meantime, the Government remains committed to reforming adult social care in England, and is providing up to £2.8 billion in 2023-24 in England and £4.7 billion in 2024-25 to put the social care system on a more sustainable footing.
September 2023
Mental Health Helpline
Selaine’s response:
I am aware that NHS England specifically sought views on the creation of a separate number for mental health from patients, clinicians and commissioners implementing local services, as well as other national mental health bodies and charities.
To achieve the ambition of a single national three digit number for mental health, stakeholders concurred that rather than creating a separate access point, we should seek to make the current main access points fit for purpose for people with urgent mental health needs. The NHS Long Term Plan commits to ensuring a significant expansion of urgent and emergency mental health care and access to these services via NHS 111.
Within the NHS 111 service, technical developments have been undertaken to ensure the mental health option is offered to callers at the earliest opportunity. These developments will go live for those areas with Mental Health Crisis lines linked via NHS 111 by March 2023, thus improving the wait time for connection to the specialist crisis mental health point of access.
September 2023
Palantir
Selaine’s response:
I understand there are some concerns over media reports about the awarding of contracts for the proposed Federated Data Platform (FDP), a new data tool to connect and integrate patient and other data sources from across the health system. The FDP will be procured via open competition, in line with Public Contracts Regulations 2015. The procurement process is open to all suppliers and will abide by the core principles of the 2015 Regulations, including transparency, non-discrimination, equal treatment and proportionality. These principles apply to all suppliers bidding for the FDP. The contract notice and standard selection questionnaire was published on 10 January, and stage 2 of the procurement was launched on 21 February.
On 20 June 2023, NHS England published a new 12 month contract to support the successful transition from the current Palantir Foundry platform to the new Federated Data Platform and Associate Services (FDP-AS) supplier. This is to provide the safe and smooth transition and exit service of critical products that were developed to respond to the Covid-19 pandemic (for Covid-19 and elective recovery purposes), to alternative provisions including the transition of products to the new FDP-AS supplier following completion of the procurement process and contract award.
All NHS contracts are procured using correct procedures. This is a new transition contract with Palantir, with new and improved contract terms, including robust exit and transition schedules to support transition from Palantir to the new federated data platform supplier. This contract includes additional terms, such as termination for convenience and a six month break clause. The contract was procured by a compliant and transparent direct award tender process, using a Crown Commercial Service framework agreement.
NHS England is committed to transparency on the way data is used within the FDP to ensure that patients are informed of the choice to opt out, where applicable and how to do so. It is also committed to publishing information on who is accessing data and for what purpose. There must always be a valid lawful basis for the collection and processing of personal information, with transparency about the use of data within the FDP, as defined under the applicable legislation.
August 2023
Smoking
Selaine’s response:
As the single leading behavioural cause of preventable death across our country, responsible for around 64,000 premature deaths per year, reducing smoking is crucial for ensuring we live longer, healthier lives.
The Government has made significant progress in this area with smoking rates the lowest on record, currently at 13 per cent, thanks to duty on cigarettes being doubled since 2010 and continued funding of stop smoking services. This year, £35 million has been committed to the NHS so that all smokers admitted to hospital will be offered NHS funded tobacco treatment services.
As part of a world first national scheme, almost 1 in 5 of all smokers in England will be provided with a vape starter kit alongside behavioural support to help them quit the habit. Later this year, local authorities will be invited to establish a scheme which suits local needs, including deciding which populations to prioritise.
The Government intends to publish a Major Conditions Strategy, recognising that reducing smoking will be central to tackling the risk of heart disease, heart attack, stroke and the cause of seven out of ten cases of lung cancer. A call for evidence to gather views on how to tackle these risk factors has recently concluded, and the strategy will be published in due course.
I am aware that charities like Action on Smoking and Health and Cancer Research UK have called for the Government to introduce a Smokefree Fund that would place a levy on tobacco manufacturers to increase funding for tobacco control programmes.
However, decisions on taxation policy are made by the Treasury. I understand that the Treasury previously consulted on introducing a levy on tobacco manufacturers and imports in 2015. At that time, the Government decided not to introduce a levy, but all taxes are kept under constant review. It is worth noting that in 2021-22, £10.3 billion of tax revenue was generated from sales of tobacco.
Minister for Primary Care and Public Health, Neil O'Brien MP has recently stated, the Government is committed to funding a range of initiatives to help people to stop smoking and/or switch to vaping. This includes providing funding for local authority stop smoking services through the Public Health Grant.
August 2023
Support for People With Terminal Illnesses
Selaine’s response:
When someone is facing the end of their life, it is vital that they receive the support they need quickly. That is why the Special Rules for End of Life (SREL) provide simple and fast access to benefits for people with a terminal illness or limited life expectancy.
I know supporting those nearing the end of their lives is a priority for the Government, and the Department for Work and Pensions (DWP) conducted a wide ranging evaluation that considered the views of claimants and clinicians on how it supports those nearing the end of their lives. Prior to this evaluation, the SREL allowed claimants who are unlikely to live longer than six months to claim under a fast tracked process without the requirement for waiting periods or a face to face assessment and, in most cases, to receive the highest rate of award.
Following the evaluation, the Government announced that the six month period would be extended to twelve months. The twelve month approach mirrors the current definition of end of life used across the NHS and ensures that people receive vital support through the Special Rules six months earlier than they did previously, reducing the need for clinicians to have multiple difficult conversations with people nearing the end of their lives
The following benefits allow claims to be made under the SREL; Personal Independence Payment, Employment and Support Allowance, Universal Credit, Disability Living Allowance and Attendance Allowance. A claim made under the SREL is generally supported by a short form, completed by a hospital consultant, GP or specialist nurse.
Changing the rules for Attendance Allowance, Disability Living Allowance and Personal Independence Payment needed new legislation. This was delivered through the Social Security (Special Rules for End of Life) Act, which received Royal Assent in October 2022. These changes mean thousands of people nearing the end of life are able to claim fast track financial support from the benefits system.
July 2023
NHS Privatisation
Selaine’s response:
The Government is clear that the NHS will always provide healthcare free at the point of delivery, regardless of ability to pay. This principle applies whether NHS funded care is being delivered by an NHS, voluntary or independent healthcare provider.
Under the NHS Constitution, patients have “the right to access certain services commissioned by NHS bodies within maximum waiting times, or for the NHS to take all reasonable steps to offer you a range of suitable alternative providers if this is not possible.”
As we seek to reduce the treatment backlog built up during the Covid-19 pandemic, independent providers have a valuable role to play in reducing NHS waiting times, by allowing patients to be treated in a private healthcare setting whilst being funded by the NHS, freeing up capacity in NHS hospitals.
The Government is ensuring the NHS has the investment it needs to deliver better care for patients, providing an extra £45.6 billion in funding for health and social care to 2024-25. As set out in the 2021 Spending Review, NHS England’s day-to-day budget is set to grow by 3.8% on average up to 2024/25, supporting the NHS to tackle the treatment backlog, and deliver its Long Term Plan. A further £2.8 billion in funding has been provided to support adult social care and discharge.
In addition, the Government is making the largest health capital investment in a decade, including the hospital rebuilding programme, and funding for new community diagnostic centres, surgical hubs and mental health urgent and emergency care facilities.
Procurement and commissioning processes are vital to ensuring that the NHS can provide the best possible care, including the adoption of innovation and efficiency. The Health and Care Act 2022 made changes to the requirement for local health bodies to competitively tender for some health care services “where it adds no or limited value”.
July 2023
NHS Digital and Patient Data
Selaine’s response:
Technology is playing a central role in realising the NHS Long Term Plan, helping clinicians use the full range of their skills, reducing bureaucracy, stimulating research, and enabling service transformation. Technology allows people to have more control over the care they receive and more support to manage their health, to keep themselves well and better manage their conditions, while assisting carers in their vital work.
The Government is committed to advance the use of digital technology in health and social care while maintaining the highest standards of privacy and ethics.
NHS Digital functions legally transferred to NHS England on 1 February 2023. NHS England is consequently responsible for ensuring it meets its obligations to protect people’s data. Data protection law will continue to apply. This means there must always be a valid, lawful basis for the collection and processing of personal information including special category information within federated data platforms and any other NHS England IT system, as defined under data protection legislation. Data protection impact assessments must be carried out and privacy notices published which explain what data is collected, analysed and shared and for what purposes.
In May, the Department of Health and Social Care published its guidance that sets out how NHS England will protect patient data, following the transfer of NHS Digital’s responsibilities. The guidance is available here: https://www.gov.uk/government/publications/nhs-englands-protection-of-patient-data.
NHS England is also legally required to report annually to Parliament on how well it has discharged its data functions. NHS England also makes an annual Data Security and Protection submission which demonstrates how they meet data protection obligations.
The Government published its strategy Data Saves Lives: Reshaping Health and Social Care with Data in June last year. This set out how digital capabilities will enable health and social care to be delivered in a much faster and more effective way, and with a greater emphasis on personalised care. This strategy is supported by the Government’s Plan for Digital Health and Social Care which outlined a £2 billion investment to digitise the NHS and at least £150 million to support digital transformation in social care.
The Government is also enabling frontline clinicians to deliver care efficiently, effectively and safely through Electronic Patient Record (EPR) systems. By December 2023, 90 per cent of NHS trusts should have EPRs in place and 100 per cent by March 2025. In September 2022, the Government published its Our Plan for Patients strategy. This committed to using joined up data and digital tools to increase patient choice and operational productivity. It also committed to freeing-up time to allow carers to care by using IT to reduce bureaucracy.
NHS England is committed to transparency on the way data is used within the FDP to ensure that patients are informed of the choice to opt out, where applicable and how to do so. It is also committed to publishing information on who is accessing data and for what purpose. There must always be a valid lawful basis for the collection and processing of personal information, with transparency about the use of data within the FDP, as defined under the applicable legislation.
July 2023
Cancer Treatment
Selaine’s response:
I am very grateful to Macmillan Cancer Support and the work of campaigners like you to raise awareness among MPs of the issues facing cancer patients and their families. Thank you to those constituents who have invited me to Macmillan's Coffee Morning event on Wednesday 13 September. I plan to attend the event and look forward to listening to the experiences of people with cancer, and receiving more information about cancer waiting times in North Devon.
I share the urgency that we reduce the backlog of cancer care that built up during the pandemic. The Government is investing £8 billion to 2025 to help deliver nine million checks, scans, and operations by 2025, and expand the number of surgical hubs across the country. I recently led a Westminster Hall debate on accessibility of radiotherapy especially in rural areas such as North Devon where were ranked 4th worse nationally for access to cancer treatment. I highlighted to the Health Minister, Will Quince, to look at not only modernising and supporting radiotherapy and cancer care but ensuring that we also account for the effects of rurality to ensure that access to treatments is available for anyone regardless of their postcode. I look forward to meeting with the Minister and supporting Macmillan Cancer support on this important matter.
July 2023
Relationships and Sexuality Education (Northern Ireland) (Amendment) Regulations 2023
Selaine’s response:
Whilst education is a devolved matter, the UK Government is required, under section 9 of the Northern Ireland (Executive Formation etc) Act 2019, to implement the recommendations in the 2018 Report of the UN Committee on the Elimination of Discrimination Against Women (CEDAW) in Northern Ireland.
The report recommended the creation of “age appropriate, comprehensive and scientifically accurate education on sexual and reproductive health and rights, a compulsory component of curriculum for adolescents, covering prevention of early pregnancy and access to abortion in Northern Ireland, and monitor its implementation.” The regulations will mirror the approach taken in England with regard to education about the prevention of early pregnancy and access to abortion.
I understand and respect there will be differing views on this issue. However, this is about ensuring compliance with the statutory duty Parliament imposed on this Government in 2019.
The UK Government has only stepped in where necessary. It has been nearly four years since this was voted on in Parliament and the Northern Ireland Department of Education has had every opportunity to bring forward measures to introduce relationships and sexuality education that implement the CEDAW recommendation.
I wish to be clear that educating adolescents on issues, such as contraception and access to abortion in Northern Ireland, should be done in a factual way that does not advocate, or oppose, a particular view on the moral and ethical considerations of abortion or contraception.
July 2023
Mental Health
Selaine’s response:
The pandemic affected the mental health of people across our country, and I welcome action taken by the Government to improve relevant support and services.
Unfortunately, I am unable to attend Mind’s parliamentary event due to my prior parliamentary commitments. However, I will be sure to follow this matter closely.
As part of the five year funding offer agreed in 2019, mental health services will receive an additional £2.3 billion a year in real terms by 2023-24 enabling service expansion and faster access to community and crisis mental health services for all. The Government has committed to increase mental health spend to 8.9 per cent of all NHS funding.
As announced in the 2021 Spending Review, a new investment of £150 million will be spent on NHS mental health facilities linked to A&E to enhance patient safety. Additionally, around £300 million will complete the programme of replacing mental health dormitories with single en-suite rooms.
Almost £1 billion of extra funding in community mental health care by 2023/24 will give 370,000 adults and older adults with severe mental illnesses, including eating disorders, greater control over their care and will support them in their communities. The Government aims to grow the mental health workforce by an additional 27,000 staff by 2023/24; indeed, the mental health workforce has increased by over 8,900 full time equivalent staff in 2022 compared to 2021.
Last year, the Government pledged to expand mental health support in schools, particularly as half of related conditions take root by the age of 14. 'Our Plan for Patients' promised to boost the number of mental health practitioners in primary care and to strengthen mental health support in schools. It also commits to improve access to NHS talking therapies and to enhance community support for adults living with severe mental illnesses.
In December 2022, the Government announced £3.6 million of funding for the National Academy of Social Prescribing, an organisation which helps those experiencing grief, addiction, dementia and loneliness through community led social activities, services and opportunities with proven benefits to well being.
The Government is set to publish a Major Conditions Strategy, and mental ill health is one of the six major conditions included. This ensures that it is considered alongside other physical health conditions rather than as a standalone strategy. The Department of Health and Social Care has launched its call for evidence for the Major Conditions Strategy; the consultation is now closed, and findings will be released in due course.
Preventing and providing better support for mental ill health will certainly be part of the strategy, as well as our separate standalone Suicide Prevention Strategy. The Government recognises that the risk factors to mental ill health are often cross-society in nature and therefore require a cross-departmental approach.
I hope these improved services end the stigma surrounding mental health, offering crucial support to those who have suffered in silence for too long.
July 2023
Health and Care for Older People
Selaine’s response:
I intend to attend Age UK’s summer reception to learn about the state of health and care for older people in 2023. I also met with Age UK in Barnstaple this month and spoke with the new CEO Amanda Howard, taking a number of points from our meeting.
My ministerial colleagues and I are aware that it is becoming more common for people to spend their later years with multiple health conditions. The percentage of people aged over 65 years old with two or more health conditions is projected to increase from 54% in 2015 to 68% in 2035.
In light of this, the Government works to support the health needs of, and prevent ill health in, older people through a variety of actions. This includes the NHS Health Check, which detects people at risk of developing cardiovascular disease in later life, and an ambitious prevention agenda to tackle the most common preventable diseases among older people. For example, encouraging people in mid life to stop smoking, reduce their alcohol consumption and improve their diet to help reduce the risk of developing dementia, disability and frailty in later life.
You may be interested to know that the Government engages with a wide range of organisations on healthy ageing, and the Office for Health Improvement and Disparities is taking targeted actions to tackle the most common preventable diseases, improving access and uptake of prevention services, and embedding prevention across health and care.
To further support the health of older people, the Government will be publishing a Major Conditions Strategy which will set out a strong and coherent policy agenda that sets out a shift to integrated, whole person care. The Strategy will tackle conditions that contribute most to morbidity and mortality across the population in England including cancers, cardiovascular disease, including stroke and diabetes, chronic respiratory diseases, dementia, mental ill health and musculoskeletal conditions. An interim report will be published in the summer.
I am also aware that the Government recently launched an Older People’s Housing Taskforce earlier this year. The panel will meet regularly and focus on overarching themes, including, the needs, preferences and concerns of older people, their families, and their carers, maximising the potential of technology, building design, and regulation to ensure homes are suitable for the future and understanding what needs to happen at the local level to enable progress in increasing the volume and diversity of housing options for older people. The taskforce will run for up to 12 months, producing an independent report to Government when it concludes.
July 2023
Dementia
Selaine’s response:
I welcome that the Government has announced its intention to develop and publish a Major Conditions Strategy. The strategy will set out a strong and coherent policy agenda that sets out a shift to integrated, whole person care. Interventions set out in the strategy will aim to alleviate pressure on the health system, as well as support the Government’s objective to increase healthy life expectancy and reduce ill health related labour market inactivity. Dementia is one of the six major conditions included in the strategy.
I have supported Alzheimer’s Society during Dementia Action Week and it was eye opening about the diagnosis rate in North Devon which is 54.4% and the steps we can take to reduce regional inequalities. I will continue to work closely with the charity to ensure that people in North Devon have a good diagnosis experience. I am aware that the Government is analysing responses and will respond shortly.
June 2023
Rare Conditions
Selaine’s response:
In 2021, the UK Rare Diseases Framework was published to set out a vision for improving outcomes for people with rare diseases. The Framework set out four priorities around delivering earlier diagnosis, increasing awareness among healthcare professionals, improving access to specialist treatment and providing coordinated care.
England’s first rare Disease Action Plan followed in 2022, which turned the priorities of the framework into concrete actions. The Government, through work across the health care sector and with the rare diseases community, has made significant progress. However, there is still more to do. The Government has published its England Rare Diseases Action Plan 2023 to further improve the lives of those living with rare diseases. It will continue to work to reduce health inequalities faced by people living with rare diseases, lower barriers to participation in clinical research and improve the way services are commissioned in NHS England.
These commitments are supported by funding for ground-breaking research, including £790 million investment into Biomedical Research Centres and a £12 million UK Rare Disease Research Platform.
I am grateful for the work of patient groups like Ehlers-Danlos Support UK and the Hypermobility Syndrome Association to support people living with these conditions.
Moving forward, the Government will continue to work closely with the delivery partners and the rare disease community to monitor progress and drive change. I will continue to follow this issue closely.
May 2023
Neurological Conditions
Selaine’s response:
I understand that there are over 600 known neurological conditions, ranging from sudden onset conditions, through intermittent and unpredictable conditions and progressive conditions to stable conditions. In November 2021, the Government announced an additional £375 million of investment over the next five years to improve our understanding and treatment of a range of neurodegenerative conditions.
Given the impact of neurological conditions, the former Prime Minister, Boris Johnson,
committed to developing a cross department strategy in November 2021 to help address the issues faced by people living with acquired brain injury (ABI).
A call for evidence around the strategy took place at the start of 2022, and people affected by ABI were invited to put forward their views about what should be prioritised and included.
Issues covered in the strategy could include guidance to prevent ABI and research into the causes of ABI and I will be sure to follow developments closely. The call for evidence also sought feedback on whether other neurological conditions should be included in the strategy.
Later this year, NHS England will develop a Long Term Workforce Plan, which will include independently verified forecasts for the number of healthcare professionals required in future years. I understand that the plan will include those professions who work with patients with Parkinson’s Disease and other long-term neurological conditions.
Thank you to those constituents who have invited me to attend the #BackThe1in6 parliamentary event hosted by the Neurological Alliance on Monday 5 June. Unfortunately I was unable to attend the event due to my other parliamentary duties, but please be assured I will continue to follow this campaign closely.
May 2023
Baby Loss
Selaine’s response:
This issue unfortunately affects many people, and I offer my sympathy to those who have suffered miscarriages, stillbirths, or the loss of a child. I applaud my colleagues who have recounted this painful experience in their lives in Parliament to raise awareness of baby loss and inspire changes in policy.
Unfortunately, I am unable to attend the Saving Babies’ Lives Progress Report launch due to parliamentary business. However, I would be interested to receive more information about baby loss and maternity care.
The UK is one of the safest places in the world to give birth. However, I know that the Government recognises that there is still more to be done. The Department of Health and Social Care has set out a range of measures to deliver its ambition to halve the rates of stillbirths, neonatal deaths and brain injuries that occur during or soon after labour, and maternal deaths by 2025 relative to levels in 2010.
I welcomed the publication of the Women's Health Strategy in July 2022 that made several commitments related to baby loss and maternity care. This included a pledge to introduce a pregnancy loss certificate in England as recommended by the interim update of the independent Pregnancy Loss Review. The Government is working to deliver these commitments to make the NHS the best place in the world to give birth through personalised, individualised, and high quality care.
May 2023
Mencap Campaign
Selaine’s response:
Patient safety and care for those with autism and learning disabilities should be to the highest standard and I am deeply concerned at the abuse that patients in Winterbourne and other hospitals faced.
Since 2015, the number of people in inpatient care has reduced by almost a fifth, which is welcome progress. The NHS Long Term Plan proposed key changes to inpatient units for those with learning disabilities and autism.
This includes commitments to reduce the number of admissions and decrease the amount of time spent in these units by 2024. I was also pleased to see these commitments renewed in the Autism Strategy (published in 2021). This will enable more people to receive personalised care in the community, closer to home, and reduce preventable admissions to inpatient services.
I fully share the concern that people with autism are still being admitted to these units. The Autism Strategy committed to improving the identification and diagnosis of autism when patients are admitted into inpatient care.
Changes are also being brought forward to the Mental Health Act 1983 to ensure that autistic people are only admitted to inpatient mental health settings if absolutely necessary. These changes would mean that autism alone is no longer a lawful basis for ongoing detention in inpatient care and would enable people in inpatient care to be discharged as soon as they are well enough to leave. A draft Mental Health Bill, which contains these proposals, has recently completed pre legislative scrutiny by backbench MPs. The Government is considering the recommendations made by MPs and will introduce the Bill when parliamentary time allows.
The Government remains committed to significantly reducing the number of people with a learning disability and autistic people in mental health hospitals. However, I recognise that there is much more to be done to reach the target set for March 2024. In the meantime, I know that the Government is working with NHS England to implement the findings of the Action Plan, including work to check that people with a learning disability and autistic people in mental health inpatient care have received a safe and wellbeing review.
May 2023
Fertility Treatment Access
Selaine’s response:
In England, decisions about local NHS fertility services are determined locally, taking account of National Institute for Health and Care Excellence (NICE) fertility guidelines. Local NHS bodies are expected to commission fertility services in line with the NICE guidelines so that there is equal access across England.
The existing NICE fertility guidelines include provisions for same sex couples who have demonstrated their clinical infertility through six failed cycles of artificial insemination. If this is the case, these couples are offered a further 6 cycles of unstimulated intrauterine insemination before proceeding to IVF. The criteria in the guidelines were developed as a way of achieving equivalence between opposite sex and same sex couples in establishing clinical infertility and accessing NHS fertility treatment services.
However, NICE has begun a review of these guidelines which will consider whether the current recommendations for access to NHS funded treatment are still appropriate. This is expected to be ready in 2024.
I wholeheartedly agree that no couple should face disproportionate or unequal costs in their efforts to overcome fertility issues. I am glad that NICE is reviewing the existing guidelines. The Department for Health and Social Care also undertook an internal review of access to NHS fertility services last year. The review informed the Government's Women’s Health Strategy published in July 2022.
The Women’s Health Strategy also outlined several ten year ambitions including a commitment to work with NHS England to address the current geographical variation in access to NHS funded fertility services across England. it also committed to ensuring that same sex couples are able to access NHS funded fertility services in a more equitable way.
May 2023
Dignity in Dying
Selaine’s response:
Thank you to those constituents who have contacted me about the Dignity in Dying event in Parliament on 23 May.
This is an issue which is greatly important to me and I am aware it is also of great importance to a number of my North Devon constituents, and I am therefore planning to attend the event.
May 2023
Dementia Diagnosis and Research
Selaine’s response:
I was very pleased to visit the Alzheimer’s Society stand at party conference last year and am eager to keep updated on the society's activities.
An estimated one million people will be living with dementia by 2025, so research is crucial to understanding the condition and improving outcomes for those affected. I was proud to stand on a manifesto that committed to doubling dementia research funding and finding a cure for dementia.
In memory of the late Dame Barbara Windsor, the Government launched a new mission in August 2022 to put this into practice. Research funding for dementia will rise to a total of £160 million a year by 2024, with an additional £95 million being provided to increase clinical trials and research projects.
A new taskforce, made up of industry, the NHS, academia and families affected by dementia, will help lead this work to allocate funding. You can register your interest to take part through the Join Dementia Research website here: https://www.joindementiaresearch.nihr.ac.uk/
Finally, the Government has announced its intention to develop and publish a Major Conditions Strategy. The Strategy will set out a strong and coherent policy agenda that sets out a shift to integrated, whole person care. Interventions set out in the Strategy will aim to alleviate pressure on the health system, as well as support the Government’s objective to increase healthy life expectancy and reduce ill health related labour market inactivity. Dementia is one of the six major conditions included in the Strategy.
May 2023
Catch Up With Cancer Campaign
Selaine’s response:
I share the commitment of the campaign to see waiting lists for cancer treatment and care significantly reduced over the next few years.
Over the last year, the Government has provided funding to help recover cancer services, and a plan that outlines how that funding will be spent effectively.
Through the NHS Long Term Plan, an additional £32 million was provided for radiotherapy equipment in 2021/22, ensuring that approximately 100 radiotherapy treatment machines could be replaced or upgraded. Reinforced by £6 billion of capital investment in the 2021 Spending Review, the NHS is gradually reducing the number of linear accelerators aged 10 years or over.
It is right that this funding comes with high expectations for reducing cancer waiting times. By March 2024, the NHS has set an ambition for 75 per cent of patients who have been urgently referred by their GP for suspected cancer to be diagnosed or have cancer ruled out within 28 days.
The Government recognises that tackling major conditions that cause ill health, including cancer, provides an opportunity to improve the lives of millions of people. That is why a Major Conditions Strategy will be developed and published over the next year to outline how outcomes in six major condition areas will be improved, including all cancers.
In the meantime, I also understand that payment arrangements for radiotherapy are being reviewed to ensure providers can increase access to new treatments and upgrade and replace equipment. These arrangements are expected to be in place from April 2023. I am personally campaigning to secure radiotherapy services in North Devon.
I was pleased to be able to attend the #CatchUpWithCancer Westminster Hall Debate on the Future of Cancer Care on Tuesday 14 March event and valued the opportunity to understand more about what steps are needed to reduce the cancer care backlog.
April 2023
GP Recruitment and Retention
Selaine’s response:
I know that the Government remains committed to increasing the number of doctors in general practice and is determined to deliver this as soon as possible. The number of GP training places has increased, with 4,032 trainees accepting a place in 2022, compared to 2,671 in 2014.
Work is ongoing with NHS England, Health Education England and the profession to increase recruitment, address the reasons why doctors leave the profession and encourage them to return to practice.
The updated GP Contract Framework announced a number of new retention schemes alongside continued support for existing schemes for the general practice workforce. In areas where there are GP vacancies, the Targeted Enhanced Recruitment Scheme provides a £20,000 salary supplement to attract GP trainees.
The Government is also taking steps to support the recruitment of GPs from overseas. In 2020, the Home Office launched the Health and Care Visa, with the aim of making it easier, cheaper and quicker for health workers, including GPs, to be recruited in the NHS.
To increase the workforce further, GP surgeries are being encouraged to become approved Home Office approved sponsors, helping more international medical graduates to be retained as GPs.
As part of the Autumn Statement, I welcomed the Government's announcement that a NHS workforce plan will be developed to consider how many staff will be required over the next 15 years to meet patient need, including General Practice.
NHS England has made a number of recruitment and retention schemes available to boost the GP workforce. This includes the GP Retention Scheme, the GP Retention Fund, the National GP Induction and Refresher, the Locum Support Scheme, and the Supporting Mentors Scheme.
As announced in the 2023 Spring Budget, the Government is also increasing the annual allowance from £40,000 to £60,000 per year to encourage GPs to work more hours. The Government is also abolishing the lifetime allowance entirely so pension tax charges do not act as a driver for early retirements.
My understanding is that the Government will launch a recovery plan for general practice in the coming weeks, which will focus on supporting GPs through providing them with the technology and tools that will help them deal with ever increasing demand.
April 2023
Parkinson's Disease
Selaine’s response:
I strongly believe that we must support the more than 120,000 people with Parkinson’s disease to access the necessary treatment, care and services to live a fulfilling, independent life.
I can fully appreciate the impact of delays in treatment and care on people living with Parkinson’s Disease caused by the pandemic. The Government is committed to tackling this backlog of care, with £5.9 billion funding for the NHS announced as part of Spending Review 2021.
Access to high quality adult social care is crucial for the effective care of people living with Parkinson’s disease and other long-term conditions. The Government’s Social Care White Paper includes proposals to increase Disabled Facilities Grants and improve access to aids and adaptations to support people to live independently in their own homes.
Research into Parkinson’s disease is vital to improving understanding more about the condition and discovering new treatments that can improve quality of life. I applaud the work of Parkinson’s UK in investing over £100 million in research to support new discoveries, develop new treatments and fund clinical trials.
As part of the Autumn Statement, the Government commissioned NHS England to develop a long term workforce plan for the NHS workforce for the next 15 years. The report, which will be published in 2023, will look at the mix and number of staff required across all parts of the country, and the actions needed to improve retention.
World Parkinson's Day provides an important opportunity to highlight issues affecting people living with Parkinson's Disease, and I am grateful to Parkinson's UK for their tireless advocacy and support for those affected and their families, including in North Devon.
Finally, I plan on attending Parkinson's UK's drop in event for World Parkinson's Day providing my other Parliamentary duties allow.
March 2023
NHS Privatisation
Selaine’s response:
The Government is clear that the NHS will always provide healthcare free at the point of delivery, regardless of ability to pay. The use of independent providers and the voluntary sector have historically played a role in the delivery of NHS services, including under the previous Labour government.
The most important way to support the delivery of care in the NHS is through investment. The Government is investing an extra £45.6 billion in funding for health and social care over the next three years, delivering better care for patients. As set out in the 2021 Spending Review, NHS England’s day to day budget is set to grow by 3.8% on average up to 2024/25, supporting the NHS to tackle the elective backlog, deliver its Long Term Plan and ensure it has the resources needed to fight Covid-19.
The Government is also making the largest health capital investment in a decade, making a real difference to the lives of NHS staff and patients, including the hospital rebuilding programme, new community diagnostic centres and mental health urgent and emergency care facilities.
I strongly dispute the claims being made in this campaign about the use of private and independent healthcare providers to deliver NHS care. Even the authors of the University of Oxford study themselves note in their conclusion that: “our findings should not be interpreted as necessarily showing a causal relationship between outsourcing and mortality rates.”
I am proud to support a Government that is committed to improving standards of patient safety, wherever NHS or independent sector care is provided. This has included establishing the Healthcare Safety Investigation Branch to investigate patient safety concerns, including care at private or independent healthcare provider settings.
Procurement and commissioning processes are vital to ensuring that the NHS can provide the best possible care, including the adoption of innovation and efficiency. The Health and Care Act 2022 made changes to the requirement for local health bodies to competitively tender for some health care services “where it adds no or limited value”.
March 2023
Ambulance Workers and NHS Pay
Selaine’s response:
Please be assured that the Government fully recognises the cost of living pressures facing ambulance workers, and this is reflected in decisions about pay increases.
The Government makes decisions on annual pay increases for ambulance workers based on the expert advice of the independent NHS Pay Review Body. In making their recommendations, the NHS Pay Review Body considers a range of factors including the cost of living, recruitment and retention.
I am encouraged to hear that Unite, Unison and the GMB have called off planned strike action, opening the path to negotiations with the Government and NHS Staff Council to find a fair and reasonable settlement. The talks will focus on pay, terms and conditions and productivity enhancing reforms. I know that the Government will continue to work towards a settlement that recognises the vital role ambulance workers have in delivering care in the NHS.
March 2023
NHS Digital and Patient Data
Selaine’s response:
Technology is playing a central role in realising the NHS Long Term Plan, helping clinicians use the full range of their skills, reducing bureaucracy, stimulating research, and enabling service transformation. Technology allows people to have more control over the care they receive and more support to manage their health, to keep themselves well and better manage their conditions, while assisting carers in their vital work.
The Government is committed to advance the use of digital technology in health and social care while maintaining the highest standards of privacy and ethics.
I note there are some concerns over media reports about the awarding of contracts for the proposed Federated Data Platform (FDP), a new data tool to connect and integrate patient and other data sources from across the health system. The FDP will be procured via open competition, in line with Public Contracts Regulations 2015. Once launched, the procurement process will be open to all suppliers and will abide by the core principles of the 2015 Regulations, including transparency, non-discrimination, equal treatment and proportionality. These principles apply to all suppliers bidding for the FDP.
NHS England is committed to transparency on the way data is used within the FDP to ensure that patients are informed of the choice to opt out, where applicable and how to do so. It is also committed to publishing information on who is accessing data and for what purpose. There must always be a valid lawful basis for the collection and processing of personal information, with transparency about the use of data within the FDP, as defined under the applicable legislation.
The Government published its strategy Data Saves Lives: Reshaping Health and Social Care with Data in June this year. This set out how digital capabilities will enable health and social care to be delivered in a much faster and more effective way, and with a greater emphasis on personalised care. This strategy is supported by the Government’s Plan for Digital Health and Social Care which outlined a £2 billion investment to digitise the NHS and at least £150 million to support digital transformation in social care.
The Government is also enabling frontline clinicians to deliver care efficiently, effectively and safely through Electronic Patient Record (EPR) systems. By December 2023, 90% of NHS trusts should have EPRs in place and 100% by March 2025. On 22 September 2022, the Government published its Our Plan for Patients strategy. This committed to using joined-up data and digital tools to increase patient choice and operational productivity. It also committed to freeing-up time to allow carers to care by using IT to reduce bureaucracy.
March 2023
Children and Young People’s Mental Health
Selaine’s response:
Living through the pandemic has had a significant impact on the mental health of people across our country, particularly children and young people, so I strongly welcome the steps the Government is taking to improve access to mental health support and services.
The NHS Long Term Plan increased investment in mental health services by at least £2.3 billion a year by 2023/24 so that an additional 345,000 children and young people are now able to get the necessary NHS funded mental health support.
In 2021/22, the Government provided an additional £79 million in response to the pandemic to expand children’s mental health services in the 2021/22 financial year. Over 689,000 children and young people under 18 were supported through NHS funded mental health community services with at least one contact in the twelve months to July 2022, compared to 615,000 for the same period to July 2021.
Mental health support teams now cover 26% of pupils in schools, a year earlier than originally proposed in the Transforming Children and Young People’s Mental Health Provision Green Paper. This will increase to 399 teams, covering around 35% of pupils by April 2023, with over 500 planned to be up and running by 2024. Rollout of further mental health support teams is being developed and will be confirmed in due course.
On average, each mental health support team will work with around 8,000 children across 10-20 schools and colleges. All schools involved will have a mental health lead. Each mental health support team is made up of education mental health practitioners and senior clinicians or higher level therapists as well as a team manager and some admin support. The teams act as a link with local NHS children and young people’s mental health services.
In Our Plan for Patients published in September last year, the Government committed to expanding mental health support for children at school, given that half of mental health conditions take root by the age of 14. This included a commitment to boost the number of mental health practitioners in primary care and to strengthen mental health support in schools. Furthermore, the Department for Education has committed to offer all state schools and colleges a grant to train a senior mental health lead by 2025, and over 10,000 schools and colleges have taken up the training offer so far.
I am planning to attend the YoungMinds event in Parliament to learn more about young people’s mental health.
March 2023
World Cancer Day
Selaine’s response:
Due to my commitments as member of the Work and Pensions Select Committee, I was unable to attend the drop in event in person however a member of my team attending in my place. The Cancer Research team sent over the statistics for North Devon and I recognise that there is a lot for us to improve to tackle waiting times and the cancer backlog.
Nevertheless, I am proud that the UK is a world leader in cancer research, and I recognise the importance of Government investment in ensuring that we can continue to improve survival and quality of life of cancer patients.
Since 2010, over £882 million in Government funding has been spent on cancer research across the UK. Ground breaking medical research is funded through the National Institute for Health Research, and spending on cancer research has risen from £101 million in 2010/11 to £138 million in 2019/20, the largest investment in a disease area.
This funding has supported research that has helped to develop new treatments and increase survival rates over the past decade in the UK.
February 2023
10-Year Mental Health Strategy
Selaine’s response:
Mental health support teams now cover 26% of pupils in schools, a year earlier than originally proposed in the Transforming Children and Young People’s Mental Health Provision Green Paper. This will increase to 399 teams, covering around 35% of pupils by April 2023, with over 500 planned to be up and running by 2024. Details on the rollout of further mental health support teams are being developed and will be confirmed in due course.
I understand there is some disappointment regarding the 10 year Mental Health Plan. However, the Government has announced its intention to develop and publish a Major Conditions Strategy. Mental ill health is one of the six major conditions included and is at the heart of the Strategy. A joined up Major Conditions Strategy instead of a standalone mental health strategy will ensure that mental ill health is also considered alongside other physical health conditions, meaning the interactions between them are reflected in the resulting plans.
Preventing mental ill health, and better supporting those with it, will be part of the Strategy, as well as our separate standalone Suicide Prevention Strategy. The Government recognises that many of the risk factors that contribute to mental ill health are cross society in nature, and it will therefore be working closely with Departments across Government.
I would like to reassure you that all the submissions received as part of the consultation on the 10 year mental health strategy will be considered as part of the Major Conditions Strategy. There were over 5,000 submissions to the mental health and wellbeing call for evidence, and the Government appreciates the engagement work many stakeholders carried out with children, young people and adults with lived experience, and more broadly, to inform their responses to the call for evidence. The Government has analysed these responses and will consider them as part of the process for developing the Major Conditions Strategy.
February 2023
Health Impacts of the Climate Crisis
Selaine’s response:
The climate crisis poses a range of challenges, not just to the UK, but to countries around the world. I appreciate concerns over the health implications of climate change. However, I would like to reassure you that the Government is working hard to reduce these impacts.
Cross departmental work is taking place to tackle some of the health implications of issues associated with climate change. Ministers have driven innovative solutions to improve air quality across a range of sectors, including funding local authorities to use innovative solutions to tackle air quality problems in their local areas through the Air Quality Grant scheme. The Government has more than doubled the funding paid to local authorities through the 2021/22 grant scheme to £11.6 million. Since 2010 more than £42 million has been awarded through the scheme, across almost 500 projects. £883 million has also been made available to affected local authorities to deliver cleaner transport and improve air quality.
To tackle the impacts of air pollution on public health, the UK Health Security Agency launched its Cleaner Air Programme to reduce people’s exposure, therefore tackling existing health inequalities, and improving outcomes for all. Furthermore, the Department for Environment Food and Rural Affairs is currently conducting a holistic review of the way the Government communicates air quality information to the public. This will ensure the public is provided with timely and relevant information about air pollution, the actions people can take to limit their personal exposure, the impacts of air pollution on their health, and their own influence on air quality. The findings of the review will support the development of future public facing air quality information.
Unfortunately, I was unable to attend the UK Health Alliance on Climate Change’s Online Briefing due to prior commitments but please be assured I will continue to follow this matter closely.
February 2023
ADHD
Selaine’s response:
I appreciate that living with neurodevelopmental conditions, like ADHD, can be difficult and I share the Government's commitment to supporting people with these conditions to live well. There is currently no waiting times for diagnosis of ADHD, and I welcome that in the recent Westminster Hall debate, the Government has committed to looking at this specifically.
In 2019, the National Institute for Health and Care Excellence (NICE) updated its existing guideline on diagnosing and managing ADHD, the quality of care and support that people receive, including access to medication.
An expert working group was established to look at how the NICE guidance and quality standards on ADHD are being implemented. It is working to identify best practice and examples of innovation, so that these can be communicated across England to improve local practice.
Further, the NHS and local authorities will develop packages to support children with neurodevelopmental disorders including ADHD and their families, throughout the diagnostic process. By 2023/24 children and young people with a learning disability, autism or both with the most complex needs will have a designated keyworker. The NHS will also roll out new waiting times to ensure rapid access to mental health services in the community for those that need it and expand crisis care.
I know that the Government recognises that there remains more to do to improve diagnosis and support for people with ADHD and I will work to ensure that this issue receives the attention it rightly deserves in Parliament.
Unfortunately I was unable to attend the Westminster Hall debate on ADHD on Monday 6 February due to my other parliamentary duties, but I welcome that issues around access to treatment will be raised in Parliament.
February 2023
Catch Up With Cancer Campaign
Selaine’s response:
I share the commitment of the campaign to see waiting lists for cancer treatment and care significantly reduced over the next few years. I recently went to the Catch Up with Cancer drop in with Radiotherapy UK in Westminster and I very much hope that further investment in radiotherapy services will help tackle cancer backlog and bring down cancer treatment waiting times.
Over the last year, the Government has provided funding to help recover cancer services, and a plan that outlines how that funding will be spent effectively.
Through the NHS Long Term Plan, an additional £32 million was provided for radiotherapy equipment in 2021/22, ensuring that approximately 100 radiotherapy treatment machines could be replaced or upgraded. Reinforced by £6 billion of capital investment in the 2021 Spending Review, the NHS is gradually reducing the number of linear accelerators aged 10 years or over.
It is right that this funding comes with high expectations for reducing cancer waiting times. By March 2024, the NHS has set an ambition for 75% of patients who have been urgently referred by their GP for suspected cancer to be diagnosed or have cancer ruled out within 28 days.
The Government recognises that tackling major conditions that cause ill-health, including cancer, provides an opportunity to improve the lives of millions of people. That is why a Major Conditions Strategy will be developed and published over the next year to outline how outcomes in six major condition areas will be improved, including all cancers.
In the meantime, I also understand that payment arrangements for radiotherapy are being reviewed to ensure providers can increase access to new treatments and upgrade and replace equipment. These arrangements are expected to be in place from April 2023.
January 2023
Hospices and the Cost of Living
Selaine’s response:
I understand that hospices are concerned about rising energy bills due to the increase of the cost of living, and note the issues raised by Hospice UK. I am assured that the Government is taking action to support hospices to ensure that they can continue to provide care to patients.
Hospices benefit from the Government's Energy Bill Relief Scheme (EBRS), which reduces how much they need to spend on their energy and gives them certainty over their budgets. In April 2023, the EBRS will be replaced by the Energy Bill Discount Scheme (EBDS) which will run until March 2024. The EBDS will support hospices by providing a discount on gas and electricity unit prices.
Hospices will receive a per-unit discount to their energy bills during the 12-month period from April 2023 to March 2024, subject to a maximum discount. The discount will be applied if wholesale prices are above a certain price threshold. For most non-domestic energy users in the UK these maximum discounts have been set at £19.61 per megawatt hour (MWh) with a price threshold of £302 per MWh for electricity, and at £6.97 per MWh with a price threshold of £107 per MWh for gas.
In addition to the Government’s support for energy bills, NHS England is supporting palliative and end of life care across the country. For example, palliative and end of life care for children and young people is being supported through the Children and Young People’s hospice grant, providing £21 million in 2022/23, rising to £25 million in 2023/24.
Furthermore, as part of the NHS Long Term Plan, up to £5 million in 2022/23 of match funding has been made available to commissioners who increase their overall level of investment in local children’s palliative and end of life care services, rising to up to £7 million in 2023/24.
I recently visited our local North Devon Hospice and was greatly impressed with the facilities, and especially the warmth and kindness of the staff there. I have taken some suggestions from the CEO back to my colleagues in Westminster and will always do everything I can do ensure our local hospice has the support necessary to continue its fantastic service.
January 2023
Dementia Diagnosis and Research
Selaine’s response:
I was very pleased to visit the Alzheimer’s Society stand at party conference this year and am eager to keep updated on the society's activities.
An estimated one million people will be living with dementia by 2025, so research is crucial to understanding the condition and improving outcomes for those affected. I was proud to stand on a manifesto that committed to doubling dementia research funding and finding a cure for dementia.
In memory of the late Dame Barbara Windsor, the Government launched a new mission in August 2022 to put this into practice. Research funding for dementia will rise to a total of £160 million a year by 2024, with an additional £95 million being provided to increase clinical trials and research projects.
I am proud that Conservative Prime Ministers from David Cameron onwards have given great priority to increasing dementia research funding, and will continue to deliver on this manifesto commitment.
A new taskforce, made up of industry, the NHS, academia and families affected by dementia, will help lead this work to allocate funding. You can register your interest to take part through the Join Dementia Research website here: https://www.joindementiaresearch.nihr.ac.uk/
This mission complements the Government’s commitment to publish the 10 Year Plan for Dementia. The 10 Year Plan plans to increase research funding for dementia and deliver a moonshot. It will focus on the specific health needs of people with dementia and their carers covering prevention, diagnosis and research. It will also look at how new technology can be used to improve outcomes for dementia patients across the country. I look forward to studying the detail of the plan in due course.
Due to the impact of the pandemic, the estimated dementia diagnosis rate fell below the national target for the first time since 2016.
While the rate has recovered slightly since the early part of the pandemic, there is more to do if we are to reach the national target for two thirds of people with dementia to be formally diagnosed.
Last year, £17 million was made available to Clinical Commissioning Groups to address dementia waiting lists and increase the number of diagnoses, which I hope will have an impact in our local area.
January 2023
Conversion Therapy Bill
Selaine’s response:
I take this issue very seriously and I know that my colleagues in the Equalities Office remain committed to tackling conversion therapy in the UK. I am absolutely clear that this practice has no place in civilised society. Being lesbian, gay or bisexual is not an illness to be treated or cured.
I am encouraged that this view is shared by the head of the NHS, the Royal College of Psychiatrists, the UK Council for Psychotherapy, the British Association for Counselling and Psychotherapy and the British Medical Association. Each of these bodies have concluded that such therapy is unethical and potentially harmful.
The Government Equalities’ Office commissioned a large-scale LGBT survey in 2017. Sadly, two per cent of respondents to the national LGBT survey said they had undergone conversion therapy in an attempt to ‘cure’ them of being LGBT. Unfortunately, in this survey, what conversion therapy entailed was not defined, nor were the respondents asked whether or not the conversion therapy referred to in their answer was offered in the UK.
As such, I welcome that the Government has delivered on its promise and introduced the Conversion Therapy Bill. I understand that the Bill will strengthen existing criminal law by ensuring that violent conversion therapy is recognised as a potential aggravating factor upon sentencing, as well as making sure those found guilty of conversion therapy offences have any profit obtained from those crimes removed. Further, it will protect freedom of speech, ensuring parents, clinicians and teachers can continue to have conversations with people seeking support. I have been assured that the legislation will not impact the existing professional frameworks that guide clinicians' ability to support people. As such, robust, exploratory and challenging conversations which are part of regulated care do not fall within the scope of the ban. It will protect under-18s regardless of circumstance and over-18s who do not consent and are forced or coerced to undergo conversion therapy practices.
I understand that the Government has now confirmed that transgender conversion therapy will be included in the ban. The Bill will be published shortly, and will protect everyone including those targeted on the basis of their sexuality, or being transgender. I am aware that this is a complex area and legislation must not harm harm the growing number of children and young adults experiencing gender-related distress, through inadvertently criminalising or chilling legitimate conversations parents or clinicians may have with their children.
I am positive about the steps that have been made so far in the UK to achieve LGBT equality, and am confident that this good work will continue.
January 2023
Every Doctor Campaign
Selaine’s response
I understand the urgency behind Every Doctor’s campaign and the challenges facing NHS staff on the frontline. I would like to take this opportunity to thank all NHS workers, including those in North Devon for their service in immensely challenging circumstances over the last two years.
Whilst I cannot commit to signing the #ReviveTheNHS pledge, I know that the Government and Health Secretary, Steve Barclay are taking steps to address the issues highlighted by the campaign to improve the experience of staff and patients in the NHS.
Given the pressures that NHS staff face daily, it is vital that everyone has access to comprehensive mental health support in their workplace.
Over the last few years, 40 dedicated support hubs have been established across the country to offer staff access to mental health services. Services can be accessed over the phone with onward referral to online and one-to-one expert help from qualified mental health clinicians, therapists, recovery workers and psychologists.
Moreover, through the Energy Bill Relief Scheme, hospitals across England will be able to receive support with energy bills this winter.
The contribution of healthcare professionals from overseas will be crucial to expanding the NHS workforce and improving access to primary and secondary care. Since the Health and Care Visa was introduced in 2020, the Government has expanded the number of occupations to help make it quicker and cheaper for healthcare professionals to work in the NHS which will help tackle the NHS backlog.
The Government is working to increase the number of GP practices registered as Home Office sponsors so that international medical graduates are able to renew their Visa while living in the UK and qualify for permanent settlement in due course.
December 2022
Abortion
Selaine’s Response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings on both sides. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion and allows Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
The approach to abortion in Great Britain is set out in the Abortion Act 1967, which states that two doctors must certify that, in their opinion, a request for an abortion meets at least one and the same ground laid out in the Act. These grounds include “risk to the life of the pregnant woman”, and “substantial risk that if the child were born it would suffer from such physical or mental abnormalities as to be seriously handicapped”.
Guidance for doctors on how to comply with the Act has been issued, which stipulates that registered medical practitioners should be able to show how they have considered the particular facts and circumstances of a case when forming their opinion. Full details can be found online at www.gov.uk/government/publications/guidance-for-doctors-on-compliance-with-the-abortion-act.
I am aware that all independent sector abortion clinics in England have been reapproved, which will ensure that abortion services continue to be available to women across the country. I understand that all current approvals are valid until 31 July 2026.
I know that making a decision regarding abortion can be extremely difficult, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all their options, with medical professionals offering impartial advice. I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion including all options available to them.
December 2022
Pancreatic Cancer Awareness Month
Selaine’s response:
I fully agree that more must be done to reduce the survival gap between pancreatic cancer and other cancers, and the development of the 10 Year Cancer Plan provides an important opportunity to focus on improving these outcomes.
Key priorities in the Plan will include supporting earlier diagnosis of cancer and increasing survival rates to match the best in Europe.
The input of patient groups like Pancreatic Cancer UK will be invaluable to help develop the 10 Year Cancer Plan by highlighting the lived experience of people with pancreatic cancer. I understand that the Plan will be published later in 2022 and the Government is currently reviewing the responses to the recent call for evidence.
Research into less survivable cancers such as pancreatic cancer is also important to improving outcomes. The Government funds research through the National Institute for Health and Care Research (NIHR), which has allocated £3.6 million towards seven research projects into pancreatic cancer since 2016.
Although this funding amounts to 5% of the NIHR’s total cancer research spending, the Government is actively encouraging more bids from researchers so that the NIHR can allocate more towards pancreatic cancer research.
Finally, thank you to those constituents who invited me to Pancreatic Cancer UK’s parliamentary drop-in event. I look forward to attending the event and hearing more about the issues affecting people living with pancreatic cancer in my local area.
November 2022
Kinship Carers
Selaine’s response:
I understand that family and friends play a vital role in caring for children who are unable to live with their parents. Quite understandably, most children benefit from living with someone they already know and trust, rather than a stranger.
I am aware that a Private Members' Bill has been tabled by Munira Wilson MP which seeks to provide a statutory definition of kinship care. Further it intends to make a provision about allowances and parental leave for kinship carers. This Government has long been committed to providing support for kinship carers, and I understand that the Department for Education is currently already considering the recommendations made in the Independent Review of Children's Social Care. This includes the recommendations to introduce a statutory definition of kinship care, provide kinship carers with paid time off work when a child starts living with them, and provide financial allowances at the same rate as foster carers.
Further, Statutory guidance for local authorities on supporting kinship carers has been issued. This makes it clear that children and young people should receive the support that they and their carers need to safeguard and promote their welfare. It explains that support, including financial support, can be provided under the Children Act 1989. Local authorities should also have clear eligibility criteria in place in relation to the support services they provide.
Local authorities are also required by central government to publish a policy that sets out their approach to promoting and supporting the needs of all children living with kinship carers. The policy should be clear, updated regularly, and made freely and widely available. I would encourage you to contact our local authority for more information about the policy in our area.
I know that the Government understands the difficulties that some grandparents face in continuing relationships with their grandchildren following disputes arising from parental separation. Work is underway to review the operation of the Child Arrangements Programme. I understand ministers will monitor how this work develops before deciding whether something specific is needed in respect of grandparents and, if so, what that might be.
I hope this reassures the constituents of North Devon that the importance and value of kinship carers in the care system is recognised.
November 2022
Pharmacy
Selaine’s response:
I would like to acknowledge the valuable and skilled work undertaken by pharmacists throughout the country every day. Community pharmacies do much more than simply dispense medicine; they play a vital role in our communities, offering advice and care.
A renewed focus on prevention has resulted in pharmacists playing a greater role in the delivery of healthcare services. To ease pressures on GP practices, the Government has committed to expanding the range of services available from community pharmacies, freeing up time for GPs to support patients with more complex needs.
The Government is committed to giving pharmacists the powers to prescribe certain medications rather than requiring a GP prescription. This position was made clear in the Government's recently published Our Plan for Patients. My colleague Therese Coffey, the Health Secretary, has stated that these measures are aimed at freeing up an estimated 2 million appointments.
The Government is also committed to sustainably funding community pharmacies. The Community Pharmacy Contractual Framework five-year deal commits £2.5 billion in each financial year between 2019 and 2024 for community pharmacies. On 22 September 2022, following discussions between the Department, NHS England and the Pharmaceutical Services Negotiating Committee, which represents pharmacy contractors in England, the Government announced an agreement for the remaining years of the Framework.
Unfortunately, I was unable to attend the Pharmacy APPG event in Parliament due to other Parliamentary duties, however, please be assured that I continue to follow this matter closely, raising it with my ministerial colleagues and working with local councillors.
November 2022
Diabetes
Selaine’s response:
Diabetes is a leading cause of premature mortality, doubling an individual's risk of cardiovascular disease. With over 22,000 additional deaths each year, it costs over £10 billion every year to manage. That is why I believe it is important that high quality diabetes care is available.
A total £5 million was provided in 2021/22 in a national recovery fund to support the recovery of routine diabetes care through innovative projects. The programme approved 28 projects with delivery continuing in 2022/23. A further £75 million of funding is also being allocated between 2020/21 and 2023/24 for the treatment and care of people living with diabetes. NHS England continues to work to identify and develop plans to address gaps in the provision of services.
The Government is, more broadly, committed to supporting the NHS to recover from the Covid-19 pandemic. An additional £23.3 billion has been announced to support the NHS in managing the ongoing impact of the pandemic. I understand that the Government is also analysing the impact of the pandemic on health conditions like diabetes, to inform how to recover the provision of routine care. I await the findings of this with interest.
Thank you to those constituents who have invited me to the Diabetes UK drop-in event on Wednesday 23 November. I regret that I cannot attend the event due to my other parliamentary duties but please be assured I will continue to closely follow this matter.
November 2022
Dementia Diagnosis and Research
Selaine’s response:
I was very pleased to visit the Alzheimer’s Society’s stand at party conference this year and am eager to keep updated on the society's activities.
An estimated one million people will be living with dementia by 2025, so research is crucial to understanding the condition and improving outcomes for those affected. I was proud to stand on a manifesto that committed to doubling dementia research funding and finding a cure for dementia.
In memory of the late Dame Barbara Windsor, the Government launched a new mission in August 2022 to put this into practice. Research funding for dementia will rise to a total of £160 million a year by 2024, with an additional £95 million being provided to increase clinical trials and research projects.
A new taskforce, made up of industry, the NHS, academia and families affected by dementia will help lead this work to allocate funding. You can register your interest to take part through the Join Dementia Research website here: https://www.joindementiaresearch.nihr.ac.uk/
This mission compliments the Government’s commitment to publish the 10-Year Plan for Dementia later this year. The 10-Year Plan will include plans to increase research funding for dementia and deliver a moonshot. It will focus on the specific health needs of people with dementia and their carers covering prevention, diagnosis and research. It will also look at how new technology can be used to improve outcomes for dementia patients across the country.
October 2022
Defibrillators
Selaine’s response:
Following the Oliver King Foundation campaign, I am glad that the Government has pledged that every school in England will have a defibrillator by the end of the 2022/23 academic year.
This will complement the requirement that has been in place since May 2020, that all contractors refurbishing or building new schools through centrally delivered programmes provide at least one automated external defibrillator (AED).
Sudden cardiac arrest (SCA) causes 100,000 deaths in the UK each year and there are 60,000 incidents of SCA each year in community settings. I know that using a defibrillator within three minutes of a cardiac arrest can improve a person’s chance of survival by as much as 70%.
That is why the NHS Long Term Plan (LTP) stated an ambition to establish a national network of community first responders and AEDs will help save up to 4,000 lives each year by 2028.
While there is no plan to mandate the location of defibrillators in Government buildings or other public places, I fully support any efforts to increase the availability and access to defibrillators, whether by local authorities, the NHS or voluntary and community organisations.
Better provision of defibrillators and increasing the number of people trained in cardiopulmonary resuscitation could help save more lives of those who have a cardiac arrest outside a hospital setting. I therefore join the Government in encouraging organisations to consider purchasing a defibrillator as part of their first-aid equipment.
Regarding the ‘Boots: save lives and install defibrillators in your stores petition, whilst I cannot commit to signing the petition, I fully support any efforts to increase the availability and access to defibrillators in our local community, including outside stores such as Boots. There are a number of funding routes available for community defibrillators, including local Councillor grants, National Lottery funding, community fundraising schemes and charities like the British Heart Foundation.
October 2022
Every Doctor Campaign
Selaine’s response:
I have been assured that my colleague Therese Coffey, the new Health Secretary, recognises the challenges facing our NHS and her priorities include reducing ambulance waiting lists and reducing the NHS backlog this Autumn.
Whilst I cannot commit to signing the EveryDoctor’s #ReviveTheNHS pledge, the Government is taking a number of actions to address the issues identified in this campaign.
I fully understand that the last two years has been a very difficult time for NHS staff, who have done an incredible job in immensely challenging circumstances.
We owe them a great debt of gratitude and I pay tribute to all NHS workers, especially those here in North Devon. I am absolutely committed, as are my colleagues, to supporting NHS staff with their mental health.
A total of 40 dedicated support hubs across the country offer staff access to mental health services. Services can be accessed over the phone with onward referral to online and one-to-one expert help from qualified mental health clinicians, therapists, recovery workers and psychologists.
I am also incredibly grateful to all those retired and partially returned staff who have returned to work for their commitment and service during the pandemic.
The suspension of the NHS Pension Scheme restrictions has been already bee extended, and I am glad that the Department of Health and Social Care has taken steps to extend the temporary retire and return easements via temporary amendments to NHS Pension Scheme regulations.
On 28 August, the Department of Health and Social Care launched a consultation on proposals to further extend the suspension of the NHS Pension Scheme restrictions until 31 March 2023. The consultation closed on 12 September. The Department is currently reviewing responses and will respond appropriately in due course.
To expand the NHS workforce during the pandemic, the Government introduced the Health and Care visa in August 2020 to made it quicker and cheaper for regulated health and care professionals to secure their visa to work in the Health and Care sector.
Furthermore, a number of Health and Care occupations, such as senior care workers, nurses and auxiliary nurses and assistants, feature on the Shortage Occupation List (SOL).
In December 2021 the Government accepted recommendations that care workers be added to the SOL, making them eligible for the Health and Care Visa.
This change came into force on 15 February 2022 and is making it easier for care employers to recruit eligible workers to reduce any staff shortages through fast-track processing and reduced visa fees.
September 2022
Palliative Care
Selaine’s response:
I believe that we must ensure that people receive the most appropriate care personalised to their individual needs as they approach the end of their life.
The NHS Long Term Plan, prepared by the NHS and published in 2019, builds on previous commitments made by the Government to personalise care through informed conversations between healthcare professionals and dying people.
Part of this is a commitment to help people to live independently for longer, as well as a promise to give more people more say about the care they receive and where they receive it, particularly towards the end of their lives. I believe empowering people with terminal conditions in this way will better enable them to access palliative care when and where they most need it.
The establishment of the Personalised Care Institute has made training available to help staff identify and support patients and to introduce personalised care planning for everyone identified as being in their last year of life. Importantly, this enables meaningful conversations to take place and allows staff to help patients and families, address their concerns and to explain the breadth of services available in the local area.
On the funding of hospices, NHS England and NHS Improvement have recently provided funding to support seven strategic clinical networks to deliver palliative and end of life care. The Health and Care Act will also require Integrated Care Boards to commission palliative care and end of life services.
August 2022
Arthritis
Selaine’s response:
I would like to assure constituents that reducing waiting times for operations required by people with arthritis, including hip and knee replacement surgery, is an urgent priority for the Government.
To date, £5.4 billion of funding has been committed to reduce the backlog of operations, including hip and knee replacements. In addition to this, the number of surgical hubs will be increased to deliver more hip and knee replacements in a COVID-secure environment.
NHS England has published a plan for the recovery of elective care in England and launched the My Planned Care platform to ensure that people waiting for treatment have access to information and support in the meantime.
It is important that local NHS bodies clearly communicate with people with arthritis on waiting lists for surgery about when they can expect to be treated, and signpost to information and support available from charities like Versus Arthritis.
To this end, I am aware that my colleague Ed Argar MP (the former Minister for Health) recently met with Versus Arthritis to discuss their ideas around the recovery of elective treatment and better understand the issues faced by people with arthritis on waiting lists.
In May the new £1.5 million Jubilee ward opened at the North Devon District Hospital using some of the money made available from the Governments catch up funding. This ward is dedicated to reducing the backlog of hip and knee surgeries and is already starting to make a difference.
Smoking
Selaine’s response:
As a leading cause of preventable death across our country, responsible for around 74,600 deaths across England in 2019, reducing smoking is crucial for ensuring we live longer, healthier lives. It is welcome therefore that the Government has set the bold ambition for England to be smoke-free by 2030.
In 2017, the Government published the latest Tobacco Control Plan. Whilst Covid-19 has disrupted some of the Plan’s delivery, a review in June 2021 found that of 82 milestones with a delivery date by 31 December 2021, 54 were already complete with the rest making progress.
As my colleague Maggie Throup, the Public Health Minister, said at the ASH Parliamentary Reception on 9 March, the Government is committed to publishing an updated Tobacco Control Plan later this year.
The revised Tobacco Control Plan will consider the findings of an independent review, led by Javed Khan, of progress towards delivering a smoke-free England.
The independent review made a number of recommendations, which included prohibiting smoking outside in hospitality venues, making hospital grounds smoke-free and reducing smoking in social housing. I understand the Government intends to consider the detail of the review in full before responding in due course.
Ministers have confirmed that they are considering a range of interventions for the plan, including those suggested by the APPG on Smoking and Health and those put forward as amendments to the Health and Care Act.
July 2022
Children In Care
Selaine’s response:
In 2021, the Department for Education launched an independent review of children’s social care, which has recently published its findings and recommendations. The review examined whole system of children’s social care including safeguarding a child’s journey into and out of the care system, as well as related features of preventative services that are provided to children and families as part of early help.
The review has said that struggling families need early intervention from local services to ensure they do not reach crisis point. The review’s recommendations include phasing out young offender institutions; a drive to recruit more foster parents; a new law to protect care leavers from discrimination; and new child-protection experts to ensure senior staff are directly involved in frontline decision-making.
I welcome the Department’s response to the review and a promise of determined change in the near future. Proposals include setting up a new National Implementation Board of sector experts and people with experience of leading change and the care system; improving efforts to recruit more foster carers increased support for social workers including on leadership, recruitment and retention; and the implementation of a new evidence-based framework for all the professionals working in social childcare. The support social workers receive in the early part of their careers will be refocused, to enhance their skills and knowledge of child protection.
Further, I am glad that seven areas of England will receive funding to set up Family Hubs which offer early help and intervention, in recognition of the importance of strong, joined up local services as a foundation for an improved social care system. Local authorities in North Devon will also receive funding for schemes that support vulnerable children to remain engaged in their education and strengthen links between social care and education. I am aware that a National Children’s Social Care Framework will also be developed, setting a direction for the system and point everyone to the best available evidence to support families and protect children.
Please be assured I will continue to monitor the progress of these ambitions to guarantee improvements to children and young people’s lives.
July 2022
Abortion (Both Lives)
Selaine’s response:
Abortion on the grounds of sex alone is illegal and guidance for doctors on how to comply with the Act makes this clear. With regard to the Non-Invasive Prenatal Test, this test is never meant to be used to determine the sex of a child, and I share your concerns that this test could be misused to inform sex selective abortion. That is why the Government will continue to review the evidence regarding the test.
The UK Government has no plans to revise the 24-week time limit for abortion. However, Parliament can propose any changes to the law on abortion. In those circumstances, the Government would take a neutral stance and allow Members to vote according to their conscience.
I am saddened to hear about findings that many women experience discrimination during pregnancy, maternity leave or after maternity leave. Under employment law, employers are required to provide minimum employment rights, including maternity leave and pay.
I know that making a decision regarding abortion can be extremely difficult, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all their options, with medical professionals offering impartial advice.
July 2022
Abortion (Northern Ireland) Regulations 2022
Selaine’s response:
I am very concerned that women and girls are still unable to access high-quality abortion and post-abortion care in Northern Ireland. The law changed more than two years ago, and abortion services should now be available as a healthcare service in Northern Ireland. Unfortunately, this is not the case. The Northern Ireland Office has extensively engaged with the Executive and Minister for Health, but they have failed to deliver.
I welcome the Government’s commitment that when establishing the legal framework for abortion that the services themselves would be delivered and overseen locally by the Department of Health and relevant health bodies in Northern Ireland, as a healthcare service. This is important as it will ensure that abortion services can be delivered in a sustainable way and become embedded into the health and social care system in Northern Ireland in the long term.
Although there has been a huge amount of pressure on health services in response to dealing with COVID-19, it does not absolve the responsibility on other important healthcare issues. As you may be aware the deadline for abortion services to be fully commissioned in Northern Ireland passed on 31 March 2022 and I support the Government’s response which has been to introduce the Abortion (Northern Ireland) Regulations 2022, which were passed by the House of Commons on 22 June.
These regulations place a further duty on the Department of Health to make abortion services available as soon as is reasonably practicable and remove the need for Executive Committee approval before services can be commissioned.
June 2022
Assisted Dying Debate
Selaine’s response:
Thank you to those constituents who have contacted me about assisted dying, and for bringing to my attention a debate on this topic which will take place in Parliament on 4 July. I understand this follows an e-petition calling for assisted suicide to be legalised receiving over 140,000 signatures. Unfortunately, I was unable to attend this debate due to other Parliamentary duties.
Coping with terminal illness is distressing and difficult both for the patient and their families. These cases are truly moving and evoke the highest degree of compassion and emotion Please be assured I will follow this debate closely, as I understand this is an important issue for many North Devon constituents.
June 2022
Breast Cancer
Selaine’s response:
Please be assured that every effort is being made to continue raising awareness of breast cancer and to improve the treatment of all those diagnosed with this disease.
I want to provide reassurance that reducing waiting times for cancer treatment, including for breast cancer, is an urgent priority for the Government. As part of the 2021 Spending Review, £2.3 billion was allocated to improve diagnostic capacity over the next three years.
The Government is committed to rolling out at least 100 Community Diagnostic Centres (CDCs), which will be new one-stop-shops for checks, scans and tests, helping those with suspected breast cancer to access earlier diagnostic tests closer to home.
In addition, NHS England and Improvement is asking local health services to focus on reducing the number of people waiting over 62 days on cancer pathways.
The Government is committed to ensuring that as many people are diagnosed to breast cancer within 28 days from GP referral. A new 10 Year Cancer Plan is being developed, with a key priority being to drive earlier diagnosis, including through meeting the FDS and joint awareness campaigns with patient groups like Breast Cancer Now.
June 2022
Carers’ Week
Selaine’s response:
Thank you to those constituents who have contacted me about Carers' Week which takes place between 6 and 12 June. I am grateful for their suggestions of a Recovery and Respite Plan for Unpaid Carers which I would be happy to discuss with my Parliamentary colleagues.
I recognise the valuable contribution made by all types carers: residential, domiciliary, paid, unpaid, many of whom spend a significant proportion of their life providing support to family members, friends and neighbours.
The Government is continuing to support the implementation of improved rights for carers, enshrined in the Care Act 2014. Carers can receive support through the Carer Element in Universal Credit and through Pension Credit and Carer's Allowance has been increased to £69.70 per week. Over the last twelve years successive changes will have provided an additional £800 a year for carers.
The Government’s Social Care White Paper outlined a number of measures to support carers including up to £25 million to kick start a change in the services provided to support unpaid carers. This could include respite, breaks and wellbeing support. The Department of Business, Energy and Industrial Strategy (BEIS) will also introduce a Carer’s Leave entitlement of five days of unpaid leave per year for eligible employees.
Local authorities are also required to undertake a Carer's Assessment for carers who require support. This may include recording a career's needs and the impact of providing care. Local authorities have a legal duty to meet a carer's needs if these are assessed as being eligible for support.
I believe that carers must receive the right support to help them carry out their caring roles. A tenth of adults in the UK provide unpaid care for a friend or family member, and these people should be supported in the invaluable work they do. Please be assured I will continue to follow this matter closely.
June 2022
Neglected Tropical Diseases
Selaine’s response:
There have been significant successes of the UK's past work to tackle Neglected Tropical Diseases (NTDs) worldwide, successes which the reception event on 8 June, ‘Ending the Neglect: Celebrating the role in beating NTDs’ is right to celebrate. It is of course important for the UK to consolidate past success with action going forward.
To this end, I am encouraged that the UK's new international development strategy, published in May, reaffirmed global health as a key priority for UK official development assistance spend. Efforts to tackle NTDs will no doubt continue to benefit from this overarching focus, as I am sure the ministerial representative from the FCDO will set out in detail at the event.
Whilst I am unfortunately unable to attend this event due to other Parliamentary duties, I will be sure to follow this matter closely.
June 2022
Dementia Action Week
Selaine’s response:
Due to the impact of the pandemic, the estimated dementia diagnosis rate fell below the national target for the first time since 2016.
While the rate has recovered slightly since the early part of the pandemic, there is more to do if we are to reach the national target for two thirds of people with dementia to be formally diagnosed.
Last year, £17 million was made available to Clinical Commissioning Groups to address dementia waiting lists and increase the number of diagnoses, which I hope will have an impact in North Devon.
May 2022
APPG Pro-Life Event - Fetal Viability
Selaine’s response:
Thank you to those constituents who invited me to the APPG Pro-Life event on fetal viability and the case for reducing the abortion time limit.
In response to a recent question in Parliament, my colleague Maggie Throup MP (Minister for Public Health) stated while that officials keep evidence on fetal viability under review, there is currently no clear consensus from the medical profession that the age of viability has reduced below 24 weeks.
Ultimately, it is a question for Parliament whether to propose any changes to the law on abortion such as gestational time limits.
Unfortunately I was not able to attend the event due to my other parliamentary duties, but I noted the position being put forward by the speaker invited by the APPG, and would be interested in more information about the evidence being presented.
May 2022
Carers Week
Selaine’s response:
I am grateful for the suggestion of a Recovery and Respite Plan for Unpaid Carers by some constituents, which I would be happy to discuss with my Parliamentary colleagues.
I recognise the valuable contribution made by carers of all kinds, residential, domiciliary, paid, unpaid, many of whom spend a significant proportion of their life providing support to family members, friends and neighbours.
I completely agree that carers must receive the right support to help them carry out their caring roles. A tenth of adults in the UK provide unpaid care for a friend or family member, and these people should be supported in the invaluable work they do.
The Government is continuing to support the implementation of improved rights for carers, enshrined in the Care Act 2014. Carers can receive support through the Carer Element in Universal Credit and through Pension Credit and Carer's Allowance has been increased to £69.70 per week. Over the last twelve years successive changes will have provided an additional £800 a year for carers.
The Government’s Social Care White Paper outlined a number of measures to support carers including up to £25 million to kick start a change in the services provided to support unpaid carers. This could include respite, breaks and well-being support. The Department of Business, Energy and Industrial Strategy (BEIS) will also introduce a Carer’s Leave entitlement of five days of unpaid leave per year for eligible employees.
Local authorities are also required to undertake a Carer's Assessment for carers who require support. This may include recording a career's needs and the impact of providing care. Local authorities have a legal duty to meet a carer's needs if these are assessed as being eligible for support.
Going forward, NHS England at a national level and Integrated Care Boards at a local level will have a duty to involve carers when care is being commissioned for their loved one. The Department for Education (DfE) will be amending the School Census to include young carers.
May 2022
GBS3 Trial
Selaine’s response:
I know that this infection can have a devastating effect for some mothers and their babies.
I am aware that The Department for Health and Social Care is working with the National Institute for Health and Care Research (NIHR), the NIHR’s Clinical Research Network and NHS England and NHS Improvement to encourage trusts to participate in the trial and mitigate any challenges which might prevent trusts from doing so.
The Excess Treatment Cost (ETC) threshold, which forms part of the mechanism to fund non-commercial research in the National Health Service, has been cited as a barrier to participation by NHS organisations. Therefore from 1 April 2022, the organisational ETC threshold was lowered from 0.01% of operating budget to 0.001% to reduce the costs of undertaking research. I will continue to follow this closely and work with our local trust.
Maternity care is a priority for Government, and it has announced an ambition to reduce stillbirths, neonatal deaths, maternal deaths and neonatal brain injuries by 50 per cent by 2025. This includes harm and death caused by GBS.
May 2022
Women's Health Strategy – Miscarriage
Selaine’s response:
This issue unfortunately affects many people and I offer my sympathy to those who have suffered miscarriages. In March 2021, the public were asked for their views on the first ever government led, Women’s Health Strategy for England. The call for evidence was launched for two reasons: firstly, to improve the way in which the health and care system responds to women’s concerns and secondly, to improve women’s health outcomes all over England, regardless of where you live.
Nearly 100,000 responses from women across the country were submitted, informing the Government’s vision for a new healthcare system. Fertility, pregnancy, pregnancy loss and post-natal support were listed as one of the six priority areas and the second most selected topic that respondents picked for inclusion in the Women’s Health Strategy.
As part of its response, the Government indicated that it would consider how to strengthen healthcare support for women and their partners affected by pregnancy loss and consider the recommendations of the forthcoming Pregnancy Loss Review. The Government has also announced that the Women’s Health Strategy would include data on miscarriages, as well as the 24/7 availability of emergency miscarriage services.
The Strategy will be published in full later this year and the Government’s ambitions will be set out in more detail with full delivery plans. Please be assured that I will be following developments closely.
May 2022
Endometriosis
Selaine’s response:
I understand that women might also have endometriosis elsewhere in the body, other than within the pelvic cavity. Feedback from topic experts, sought by NICE (National Institute for Health and Care Excellence, detailed that there is currently no evidence upon which to base recommendations on how to best diagnose and manage endometriosis outside the pelvis, including thoracic endometriosis. The experts explained that treatment in specialist centres may improve patient outcomes and facilitate evidence generation on how to manage endometriosis outside the pelvis.
I am glad that, in December 2021, NICE made an editorial amendment to the guideline section on referral for women with suspected or confirmed endometriosis to highlight that women with endometriosis outside the pelvic cavity should be referred to a specialist endometriosis centre. While I note your desire to see changes to the NICE guideline around thoracic endometriosis, I understand that NICE has said that while they do not expect to make further changes, the issue has been added to the issue log for the guideline for consideration in future surveillance, once more evidence is available
May 2022
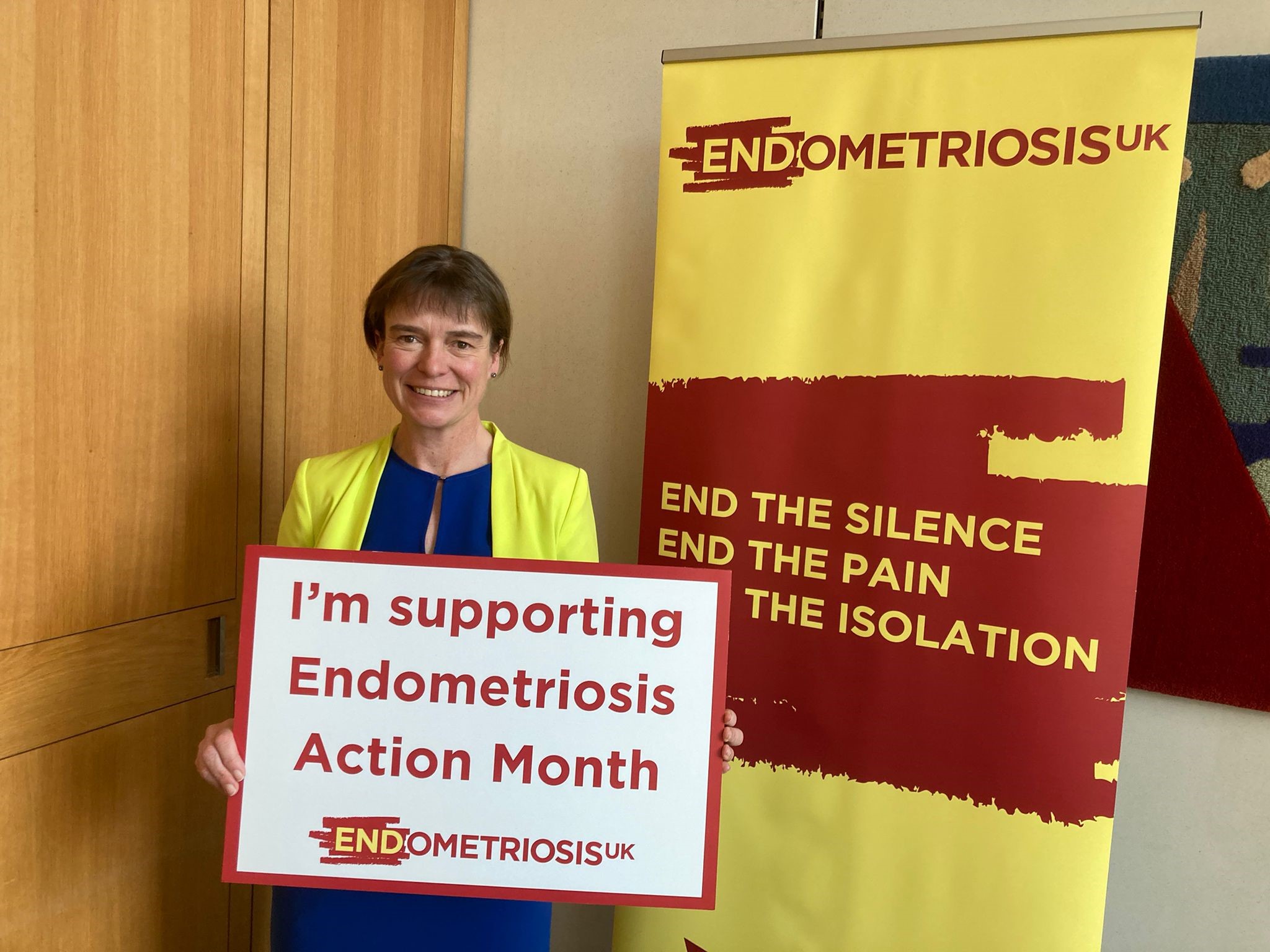
Conversion Therapy
Selaine’s response:
I am determined that everyone in the UK should be free to live their lives and fulfil their potential regardless of their sex, sexual orientation or gender identity. The LGBT community must be free to proposer in modern Britain.
I know for many in the LGBT community the issue of conversion therapy is a significant concern. I am absolutely clear that the practice of conversion therapy has no place in civilised society. Being lesbian, gay or bisexual is not an illness to be treated or cured. I understand that the Government launched a consultation on how ministers are planning to ban practices of so called 'conversion therapy'.
The consultation was extended until February 2022 to allow for ample opportunity for all those to contribute their views including faith groups, LGBT organisations, counselling bodies and charities.
I am aware that the Government is proceeding with its legislative proposals to ban conversion therapy for lesbian, gay, and bi-sexual individuals. Alongside this, I have been assured that the Government is carrying out separate work on the issue of transgender conversion therapy, this is to ensure that any legislative measures brought forward will not have any unintended consequences. I understand that this is a legally complex area, and as such the Government have a responsibility that any of these unintended consequences are not written into legislation, particularly in the case of under eighteens.
Internationally, the promotion and defence of human rights is an integral part of the UK’s foreign policy, including speaking up for gender equality and LGBT rights, and seeking an end to discrimination where it exists. The UK is clear that every country must fulfil its international human rights obligations.
As co-chair of the Equal Rights Coalition (ERC), the UK has launched the ERC's first Strategy and Five Year Implementation Plan that will increase international action to defend the rights of LGBT people around the world. Further information on the plan for 2021 to 2026 can be found at: https://www.gov.uk/government/publications/equal-rights-coalition-strategic-plan-2021-to-2026.
I am encouraged by the action of the Government to support the LGBT community in the UK and overseas. However, there is of course more that needs to be done and I will continue to press ministers to fulfil commitments made and provide further support.
May 2022
Early Medical Abortion (At Home)
Selaine’s response:
Thank you for contacting me about the provision of early medical abortion.
I completely understand that this can be an incredibly emotive issue, and can fully appreciate the strength of feeling on this matter. Given the sensitivities and as with other matters of conscience, the Government adopts a neutral stance on abortion, allowing Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
In March 2020, the Government put in place a temporary measure in England, enabling women to take both pills for early medical abortion up to ten weeks (nine weeks and six days) gestation in their own homes, following a telephone or e-consultation with a clinician, without the need to first attend a hospital or clinic. This measure was put in place to reduce the risk of transmission of Covid-19 and ensure continued access to abortion services.
Following consultation, the Government announced a six-month extension to the temporary arrangements, with the intention of returning to pre-Covid arrangements on 29 August 2022.
However, an amendment was tabled to the Health and Care Bill, currently progressing through Parliament, to reverse the Government’s decision and make permanent these temporary measures. Following a free vote, MPs voted in favour of the amendment to make the provisions permanent.
For my part, I voted against this amendment. I believe that women should have access to support and care when making this difficult decision, and I feel there would have been better ways to ensure women were provided with the necessary support. This was temporary legislation, and my opinion is that instead of making this permanent through an amendment, that we should have taken more time to properly scrutinise these changes, even if this meant bringing forward specific legislation to address this issue. In the end, the amendment was passed, and I trust that women will take great care and personal consideration for any choice they make, but would always encourage anyone making such an important decision to seek advice.
The Health and Care Bill has now returned to the House of Lords for further scrutiny and I will follow its progress carefully.
April 2022
Health and Care Bill: Workforce
Selaine’s response:
Our NHS relies on effective workforce planning to ensure we can meet the health and care needs of local communities and I applaud the dedication of healthcare professionals across a range of professions.
Clause 35 of the Health and Care Bill would require the publication of a workforce report at least every five years - covering the whole of the NHS including primary, secondary and community care.
This report will increase transparency and accountability in the workforce planning process. For example, the report would set out the role and responsibilities of new Integrated Care Boards (ICBs) about how they would ensure the delivery of effective local workforce planning.
I recognise that people would like to go further, and the level of support that an amendment made to the Bill in the House of Lords has received from Peers, patient groups and professional bodies.
However, I disagree with this amendment because I believe that the Government's clause is sufficient and it is not necessary to add further or different reporting duties on that topic. There is common ground on the need to have effective workforce planning.
As my colleague Ed Argar, the Minister for Health has stated, we cannot predict all future workforce needs, which is why the report is required to be published at a minimum of every five years.
This flexibility will allow an updated report to be provided earlier than the statutory required period to reflect any changes to roles and responsibilities.
It should be kept in mind that in addition to Government measures in the Bill, the Department for Health and Social Care has already commissioned the development of a long term, 15 year strategic framework for the health and social care workforce. This is a welcome piece of work and I look forward to its publication, which I am told is expected later this year.
It is vital that workforce planning is closely integrated to the wider planning across health and social care. Two key NHS bodies will be merged to help put long term planning and strategy for healthcare staff recruitment and retention at the forefront of the national NHS agenda.
The Government is delivering against its key pledges to increase the numbers of GPs and nurses and there are 1,200 more GPs and 27,000 more nurses compared to 2019.
I believe that the measures in the Health and Care Bill will help to clarify who is responsible for workforce planning and ensure NHS can provide the workforce needed to meet the health and care needs of the population.
April 2022
Social Care Cap (Means Test)
Selaine’s response:
I am proud to support a Government that is committed to taking the difficult decisions and tackling the problems in the social care system head on. This historic plan for adult social care will protect individuals and families from unpredictable and potentially catastrophic care costs.
From October 2023, no eligible person starting adult social care will have to pay more than £86,000 for personal care over their lifetime. To be clear, the cap is not a target to be hit, but a backstop protection to ensure people have certainty and avoid catastrophic costs. The reformed means test, which is the best way to help make care affordable, will increase the threshold above which people must meet the full cost of their care to £100,000. This is more than four times the current limit of £23,250, and the number of people receiving state support in the social care system will increase from around half to two thirds.
In designing these reforms, the priority has been the creating a more generous means-testing system, which benefits those with low to moderate wealth. The nature of the means-test will dramatically reduce the amount that less well-off users will have to spend on care. For example, someone who has £100,000 of assets would need to draw on care and support in a residential home for about 10 years to spend the same amount as someone who entirely self-funds. Older adults have around a one in three chance of living in a residential home for three years and a one in 50 chance of doing so for 10 years.
Only the amount that an individual contributes towards their personal care will count towards the cap. This ensures that individuals living in different parts of the country, but contributing the same amount, do not progress towards the cap at different rates because of differences in amounts paid by their local authorities. It is right that less well-off people in different parts of the country benefit to the same extent and we do not see differences based simply on where someone lives.
The new social care reforms are clear, fair and reduce complexity. I am proud to support a Government that is tackling the issue of social care reform head on, significantly improving the sustainability and affordability of the provision of social care.
April 2022
Diabetes
Selaine’s response:
Diabetes is a leading cause of premature mortality, doubling an individual's risk of cardiovascular disease. With over 22,000 additional deaths each year, it costs over £10 billion every year to manage. That is why I believe it is important that high quality diabetes care is available. My grandfather developed late onset, type 1 diabetes so I do have personal experience of how difficult this condition is.
NHS England has invested approximately £120 million of funding into local services to improve performance in the treatment and care of people living with diabetes since 2017/18. This is focused on improving attendance at structured education to increase understanding, improving achievement of NICE targets, reducing amputations through improved provision of multidisciplinary footcare teams, improving timelines of referrals from primary care for patients with diabetic foot disease, and reducing lengths of stay for diabetic inpatients through specialist nursing services.
It is important that people with diabetes can access the routine care and support that they need, and am glad that the Government is committed to supporting the NHS to recover from the Covid-19 pandemic. An additional £23.3 billion has been announced to support the NHS in managing the ongoing impact of pandemic. I understand that the Government is also analysing the impact of the pandemic on health conditions like diabetes, to inform how to recover the provision of routine care. I await the findings of this with interest.
I was very interested to hear of the Diabetes is Serious reception, and I am planning to attend. I am glad of the opportunity to hear directly from people living with diabetes about the impact.
April 2022
Catch Up With Cancer Campaign
Selaine’s response:
Let me assure you that I share the commitment of the campaign to see waiting lists for cancer treatment and care to be reduced over the next few years and I have ensured that ministerial colleagues are aware of the campaign and its calls to action. I am also a member of the All Party Parliamentary Group for Radiotherapy.
In recent months, the Government has brought forward funding to help recover cancer services, and a plan that outlines how that funding will be spent effectively.
Last year it was announced that nearly £6 billion is being put towards capital investment for new beds, equipment and technology. This funding will contribute towards expanding mobile diagnostics for cancer and upgrading MRI and screening technology.
The expansion of elective capacity will focus on rolling out new and innovative forms of radiotherapy to deliver treatment in a more targeted and intensive way, meaning cancer patients spend less time in Hospital.
It is right that this funding comes with high expectations for reducing cancer waiting times. By March 2024, the NHS has set an ambition for 75% of patients who have been urgently referred by their GP for suspected cancer to be diagnosed or have cancer ruled out within 28 days.
April 2022
Carer’s Allowance
Selaine’s response:
I recognise and appreciate the vital role played by unpaid carers now more than ever, and I understand that this is an extremely important issue for many carers.
The primary purpose of Carer's Allowance is to provide a measure of financial support for people who give up the opportunity of full-time employment in order to care for a severely disabled person. It must be stressed that it is not a carer’s wage or a payment for the services of caring, nor is it intended to replace lost or forgone earnings in their entirety.
The Carer's Allowance earnings limit is not linked to the number of hours worked. Instead, it is set at a level that aims to encourage people to maintain a link with the labour market through part time work. The earnings limit for Carer's Allowance is a net figure, meaning it takes into account income tax, National Insurance contributions and half of any contributions to an occupational or personal pension, and there are also a number of other deductions which can be made. That means that people can earn significantly more than £128 per week gross and still be eligible for Carer's Allowance.
In the past decade, the rate of Carer’s Allowance has increased from £53.90 to £67.60 a week, meaning nearly an additional £700 a year for hundreds of thousands of carers. This will increase further to £69.70 per week from April.
April 2022
Dementia Research and Diagnosis
Selaine’s response:
Research is crucial to understanding and tackling dementia, and I was proud to stand on a manifesto that committed to making finding a cure for dementia one of the Government's biggest collective priorities. I look forward to the publication of the dementia strategy later this year, which will focus on the specific health and care needs of people living with dementia and their carers, including dementia diagnosis and research.
The 2021 Spending Review saw £5 billion committed to health-related research and development and I understand that work is ongoing to finalise outcomes from the spending review and to identify ways to significantly boost research on dementia, which is encouraging. I was delighted by the Government's announcement in November of a £375 million investment, over the next five years, to improve understanding and treatment for a range of neurodegenerative diseases, including different types of dementia.
It is disappointing that, due to the impact of the pandemic, the estimated dementia diagnosis rate fell below the national target for the first time since 2016. While the rate has recovered slightly since the early part of the pandemic, there is more to do if we are to reach the national target for two thirds of people with dementia to be formally diagnosed. Last year, £17 million was made available to clinical commissioning groups to address dementia waiting lists and increase the number of diagnoses, which I hope will have an impact in our local area.
March 2022
Health and Care Bill: Workforce
Selaine’s response:
Our NHS relies on effective workforce planning to ensure we can meet the health and care needs of local communities and I applaud the dedication of healthcare professionals across a range of professions.
Clause 35 of the Health and Care Bill would require the production of a workforce accountability report at least every five years. This report will increase transparency and accountability in the workforce planning process. For example, the report would set out the role and responsibilities of new Integrated Care Boards (ICBs) about how they would ensure the delivery of effective local and national workforce planning.
I recognise that people would like to go further, but there is common ground on the need to have effective workforce planning.
As my colleague Ed Argar, the Minister for Health, has stated, we cannot predict all future workforce needs, which is why the report is required to be published at a minimum of every five years.
This flexibility will allow an updated report to be provided earlier than the statutory required period to reflect any changes to roles and responsibilities .
I also recognise the level of support an amendment made to the Bill in the House of Lords has received from Peers, patient groups and professional bodies. I look forward to giving further consideration to workforce planning when the Bill returns to the House of Commons later this month.
It should be kept in mind that in addition to Government measures in the Bill, the Department for Health and Social Care has already commissioned the development of a long-term 15-year strategic framework for the health and social care workforce. This is a welcome piece of work and I look forward to its publication, which I am told is expected later this year.
It is vital that workforce planning is closely integrated to the wider planning across health and social care. Two key NHS bodies will be merged to help put long-term planning and strategy for healthcare staff recruitment and retention at the forefront of the national NHS agenda.
The Government is delivering against its key pledges to increase the numbers of GPs and nurse, there are 1,200 more GPs and 27,000 more nurses compared to 2019.
I believe that the measures in the Health and Care Bill will help to clarify who is responsible for workforce planning and ensure NHS can provide the workforce needed to meet the health and care needs of the population.
March 2022
Water Fluoridation
Selaine’s response:
While I note some constituent’s concerns about fluoride in our water supply, fluoridation programmes in our country are common practice, and have been in place for nearly 60 years. I am aware that currently, around 5.8 million people in England already consume fluoridated water. I would like to reassure constituents that there have been no cases of water fluoridation causing any ill effects.
I understand that a report from Public Health England, now the Office for Health Improvement and Disparities, on improving oral health, published in 2020, found that water fluoridation significantly reduces tooth decay, especially in children. It found that, in deprived areas where water fluoridation occurs, there were 55% fewer hospital admissions for tooth decay among children aged one to four.
This scheme is effective and safe and I am reassured that there is no evidence of health harms from the levels of fluoride used in English schemes, nor the slightly higher levels allowed naturally. Further, the Government is required to monitor the effects of water fluoridation and produce reports on this every four-years, which I hope you find reassuring. The last report was published in 2018 which means that there will be a new report, which is due to be published in 2022.
While this is a government-supported programme, local authorities are responsible for any consultations on fluoridation schemes. You will be encouraged to know that ministers have published a toolkit for local authorities to aid them in carrying out these consultations. However, it is worth noting that the new Health and Care Bill proposes to return responsibility for the fluoridation of water in England from local authorities to central government, making it easier to expand water fluoridation schemes so that more of the population can benefit from it.
I know that some are concerned by previous suggestions of adverse effects from fluoridated drinking water, such as a rare form of bone cancer (osteosarcoma), Down’s syndrome or effects on the kidney. I am, however, reassured that evidence does not support this and that various authoritative expert evaluations from different international organisations all agree that there is no convincing evidence that fluoride in drinking water at levels used in fluoridation schemes or at concentrations below the regulatory drinking water limit is harmful to general health.
March 2022
Care Home Visits
Selaine’s response:
I know that throughout the pandemic, the Government has done everything it can to protect people receiving care and staff and it is vital that this continues. While the vast majority of people cared for in care homes and at home are vaccinated, the risk of transmission and hospitalisation from Covid-19 remains higher than in the general population. I am told that current protections in social care will remain and the Government continues to review all Covid-19 measures for social care in line with the latest scientific advice.
Further details of any changes will be provided in due course, and I await this with interest. I have ensured that ministers are aware of the concerns that you have raised with me.
March 2022
‘At home’ Abortions
Selaine’s response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings around this matter. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion, allowing Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
In February, the Government announced a six month extension to temporary arrangements put in place at the beginning of the pandemic that mean women can take both pills for early medical abortion at home.
The temporary approval will end at midnight on 29 August and, from this point, the pre-Covid regulatory requirements for the provision of early medical abortion will be reinstated.
These measures were put in place as part of the public health emergency, in order to address a specific and acute medical need, reducing the risk of transmission of Covid-19, and to ensure that abortion services could continue to be accessed during this unprecedented time. Like many of the other measures brought in around this time they were temporary, and time-limited to two years.
I know that the Government recognises the sensitivities around abortion, and so I am glad that they consulted thoroughly on whether to make these temporary arrangements permanent, giving everyone an opportunity to input views, evidence and data. I am told that, after careful consideration, the Government has come to the view that the provision of early medical abortion should return to pre-Covid arrangements. I am also assured that the wellbeing and safety of women requiring access to abortion services has been, and will continue to be, the first and foremost priority.
Thanks to the success of the vaccination programme, we are in a very different position compared to the beginning of the pandemic, however health services have been under increased pressure in recent months. For this reason, the six month extension has been approved to enable a safe and reliable return to pre-pandemic arrangements and continued access to services.
February 2022
Bite Back Better
Selaine’s response:
It is fantastic to see the passion of the young people who are part of the Bite Back Better campaign to promote healthier lifestyles and to reduce childhood obesity.
The Government is committed to implementing its promise to ban pre-9pm TV advertising of food high in sugar, salt and fat across the UK. Recognising that a growing number of young people consume media online, I am also delighted that the Government will also restrict paid-for-advertising online.
These restrictions are being included as part of the Health and Care Bill that is going through Parliament at the moment. I am confident that such measures will help us to reach the Prime Minister's goal of halving childhood obesity by 2030 and help adults to reach a healthy weight.
I am also pleased that the Government's Levelling Up White Paper has recognised the role of obesity in driving poor health outcomes in communities across the UK. As part of the White Paper, the Government has promised to take forward recommendations from Henry Dimbleby’s independent review towards a National Food Strategy including piloting Community Eatwell and a school cooking revolution.
February 2022
Dementia Research
Selaine’s response:
I entirely agree that research is crucial to understanding and tackling dementia, and was proud to stand on a manifesto that committed to making finding a cure for dementia one of the Government's biggest collective priorities through the dementia moonshot.
As part of the 2020 Challenge on Dementia, £344 million was spent on dementia research in the past five years and I know that the Government is strongly committed to continuing to support research into dementia, having made a number of welcome funding commitments. At the 2021 Spending Review, £5 billion was committed to health-related research and development over the Spending Review period and I hope to see dementia research benefit from this funding. Additionally, I was delighted by the Government's announcement in November of a £375 million investment, over the next five years, to improve understanding and treatment for a range of neurodegenerative diseases. This includes Fronto-temporal dementia, Parkinson’s disease dementia, Lewy Body dementia and Alzheimer’s disease, among others.
I understand the Government is currently working on ways to significantly boost further research on dementia and I am told that a new dementia strategy is expected to be published this year. The strategy will include ambitions for dementia research and increasing dementia research funding and I look forward to its publication, particularly as I am a Dementia Friend.
I welcome the opportunity for Parliament to discuss this important issue and I am sure it will be a very compelling discussion. While I am unable to speak in the debate due to prior commitments, I will ensure that ministers are aware of the points you have shared with me.
February 2022
Assisted Dying (Update)
Selaine’s response:
As a general principle, I believe that individuals should have as much control as possible over their own lives. This leads me to be broadly supportive of a change in the law to allow assisted dying for those who are terminally ill and mentally competent. We must be incredibly careful to ensure that any change in the law does not encourage anybody to make the decision to end their life. New or amended legislation should only allow those who are already determined to end their lives to do so without their loved ones having to endure difficult legal processes afterwards.
This is an incredibly difficult issue and the case studies which many constituents have highlighted are deeply saddening. However, I completely understand why other people feel equally strongly against assisted dying and their views are to be respected. It is good that these sorts of issues are almost always considered to be 'issues of conscience' when Parliament votes on them and so MPs are free from political constraints in deciding their views. Assisted dying is regularly considered by Parliament and I am sure that this Parliament will be no exception. In the case of me voting on the matter, I would take into account the stories I have heard from constituents, who too feel strongly about this emotive issue.
Thank you to those constituents who have invited me to the briefing meeting on 19th October. Unfortunately, I am unable to attend the meeting on this occasion, but I will always continue to review emerging research in this area.
Unfortunately, I am unable to attend the meeting on this occasion, but I will always continue to review emerging research in this area as I understand this is an important issue for many constituents.
February 2022
Radiotherapy
Selaine’s response:
Cancer remains a high priority for the Government and despite survival rates being at a record high, too many people continue to die from it, leaving many devastated by the loss of loved ones. In the past decade, rates of survival from cancer have increased year-on-year. Around 7,000 people are alive today who would not have been had mortality rates stayed the same as then.
The NHS Long Term Plan (LTP), published during 2019, outlined a number of new measures for catching cancer early and providing treatment, with the aim that from 2028, 55,000 more people each year will survive their cancer for at least five years after diagnosis.
One of the measures outlined in the plan is safer and more precise treatment, including advanced radiotherapy techniques and immunotherapies to continue to support improvements in survival rates.
This will be supported by a £130 million upgrade of radiotherapy machines across England, including £32 million to replace 17 Linear Accelerators aged over 10 years by the end of March 2022, as well as commissioning the NHS new state-of-the-art Proton Beam facilities in London and Manchester.
In addition, the LTP commits to reforms to the specialised commissioning payments for radiotherapy hypofractionation to support further equipment upgrades. Faster, smarter and more effective radiotherapy, supported by greater networking of specialised expertise, will mean more patients are offered curative treatment, with fewer side effects and shorter treatment times.
Starting with ovarian cancer, the NHS will ensure greater access to specialist expertise and knowledge in the treatment of cancers where there are fewer or more risky treatment options.
I hope that this provides reassurance that providing adequate support for a widely used and effective treatment for cancer is absolutely a priority for the Department of Health and Social Care and across the NHS.
January 2022
NHS Winter Preparedness
Selaine’s response:
I am reassured by the measures being put in place by the NHS, which focuses on increasing protection of the population through vaccination. This includes actions to accelerate the Covid-19 booster vaccine roll out and making sure that everyone who is eligible for a flu vaccination is able to get one.
NHS England and NHS Improvement are working with NHS providers to ensure appropriate plans are in place, including meeting potential increases in the demand for emergency care driven by seasonal flu and Covid-19.
It is welcome that the NHS will receive an extra £5.4 billion over the next six months to support its response to Covid-19. This includes £2.8 billion to cover related costs such as enhanced infection control measures and £478 million to continue the enhanced hospital discharge programme, to maintain capacity.
The Government is also taking action to increase NHS capacity so that the health service is well equipped to reduce waiting lists for operations such as hip and knee replacements. Alongside the £8 billion funding announced in the Spending Review 2021, a plan for recovering elective care will shortly be published by NHS England and Improvement.
December 2021
Conversion Therapy
Selaine’s response:
I take this issue very seriously and I know that my colleagues in the Equalities Office remain committed to tackling conversion therapy in the UK. I am absolutely clear that this practice has no place in civilised society. Being lesbian, gay or bisexual is not an illness to be treated or cured.
I am encouraged that this view is shared by the head of the NHS, the Royal College of Psychiatrists, the UK Council for Psychotherapy, the British Association for Counselling and Psychotherapy and the British Medical Association. Each of these bodies have concluded that such therapy is unethical and potentially harmful.
The Government Equalities’ Office commissioned a large-scale LGBT survey in 2017. Sadly, 2% of respondents to the national LGBT survey said they had undergone conversion therapy in an attempt to ‘cure’ them of being LGBT. Unfortunately, in this survey, what conversion therapy entailed was not defined, nor were the respondents asked whether or not the conversion therapy referred to in their answer was offered in the UK.
I very much welcome the fact that the Government is delivering on its promise and will legislate to ban conversion therapy to protect LGBT people from this harmful practice.
The Government launched a six-week consultation on how ministers plan to ban practices of so called 'conversion therapy'. The consultation was due to close on 10th December but has now been extended by eight weeks, this is to ensure that the widest possible views are being taken into account. I understand that the consultation has already taken views from members of the public, victims of conversion therapy, LGBT organisations, faith groups, psychiatric and counselling bodies, charities and other interested stakeholders to ensure we hear from all voices in shaping the ban on conversion therapy. However, the consultation will now close on 4 February, in order to allow ample opportunity for those to contribute who have not yet been able to do so. As such, I would therefore encourage you to take part at the following link:
https://www.gov.uk/government/consultations/banning-conversion-therapy
The Government's proposals include the creation of a new criminal offence and we will also ensure that conversion therapy is considered by judges as a potential aggravating factor upon sentencing for existing violent criminal offences.
Ministers further propose a range of other supportive measures including the introduction of statutory Conversion Therapy Protection Orders to protect individuals facing imminent risk, such as forced travel abroad to receive conversion therapy.
The results will be analysed and will inform the Government's next steps in preparing legislation for spring 2022.
The Equality Hub is engaging with a wide range of stakeholders who hold different views in relation to conversion therapy. Ministers have been clear that the recently launched consultation is looking into how, not whether, to ban conversion therapy. I welcome this approach to engage with everyone who has an interest in this area. I will continue to follow this closely and look forward to reviewing the Government's final proposals when they are released.
December 2021
APPG Pro-Life Event 14.12.2021 - Crisis Pregnancy Care
Selaine’s response:
Thank you to those constituents who invited me to the upcoming All-Party Parliamentary Pro-Life Group meeting on crisis pregnancy care.
According to a study in the Lancet, 45% of pregnancies and one third of births in England are unplanned or associated with feelings of ambivalence. Public Health England has previously highlighted the impact of unplanned pregnancies on the mental and physical health of both women and children.
Improving access to information, advice and services are crucial to helping women to make an informed decision around pregnancy, and supporting good reproductive health.
Unfortunately, I am unable to attend the meeting due to my other parliamentary duties, but thank you for inviting me to this event and bringing these issues to my attention.
December 2021
Abortion ('DIY Abortions')
Selaine’s response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings around this matter. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion, allowing Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
Guidelines have been issued which enable women to take both Mifepristone and Misoprostol at home for the duration of the pandemic, so that they do not have to visit a medical practice and risk exposure to the virus, and to enable doctors to prescribe medicines from home via telephone or video consultations without consulting a second practitioner, so that abortion care can be provided even in the case of staff shortages.
The medicines must still be instigated prior to nine weeks and six days into the pregnancy. I am aware of data that indicates an increase in the number of abortions carried out in 2020. The pandemic has had an impact on many aspects of daily life, the full picture of which may not be clear for some time to come. I will, of course, continue to monitor this sensitive issue.
A consultation has recently been held on the home use of both pills for early medical abortion up to 10 weeks gestation. The Government is currently reviewing the evidence received and will publish a response in due course. More information can be found here:
https://www.gov.uk/government/consultations/home-use-of-both-pills-for-early-medical-abortion
I have been distressed to read news reports of cases where abortions had been sought and enacted after the ten week legal limit for taking the medicines at home, and have caused further illness and even death. I understand that these instances are being investigated to ensure that women are accessing safe care, and that clinicians are properly supported through the consultation process. I will continue to support all efforts to ensure safety is a paramount consideration for any amendments to regulations, however temporary. I will continue to monitor this issue closely.
A decision regarding abortion care can be an extremely difficult time, and I believe that we must do all we can to support women to make an informed decision.
As my colleague Maggie Throup MP (Minister for Public Health) recently said in response to a parliamentary question, "It is important that women receive accurate and evidence-based information on abortion. The Department’s Required Standard Operating Procedures set out that women must be given impartial, accurate and evidence-based information both verbal and written, delivered neutrally by all abortion providers."
I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion care including all options available to them.
December 2021
Health and Care Bill
The unprecedented threat of the Covid-19 pandemic reminded us how vital our health and care system is to all of us. I want to assure you that the NHS will always be free at the point of use, and any proposed reforms will aim to continue to improve the quality of these services and patient outcomes.
As we build back better from this pandemic, it is right and necessary that our health and care services are at the forefront. The pandemic underlined not only the dedication and skill of those in this sector, but also the necessity of a broader, more integrated health and care system. I welcome the intention to develop more integrated care between the NHS, Local Government and other partners including the voluntary and community sector, which will be vital in tackling the factors that affect the long-term sustainability of patient services. The Bill will make permanent some of the innovations brought about by the pandemic. I understand that these proposed reforms will also include proper accountability mechanisms and give patients and the public the confidence that they are receiving the best care from their healthcare system.
The measures set out in the Health and Care Bill deliver on the NHS’s own proposals for reform in its Long Term Plan. I believe these proposals have been developed in consultation with key stakeholders in this sector, and I am encouraged by the preliminary positive feedback received. In particular, the comments from the former Chief Executive of NHS England, who said that this Bill “will support our health and care services to be more integrated and innovative so the NHS can thrive in the decades to come”, are reassuring.
Health and Care Bill: Workforce
The workforce is the beating heart of the NHS and I pay tribute to all those who work so hard in our health service.
Clause 34 of the Health and Care Bill would require the production of a workforce accountability report at least every five years. This report will increase transparency and accountability in the workforce planning process, putting in place the proper structures.
Additionally, the Department for Health and Social Care has already commissioned Health Education England to work with partners to develop a long-term 15-year strategic framework for the health and social care workforce. This will look at the key drivers of workforce demand and supply over the longer term and will set out how they impact on the future workforce. This is a welcome piece of work and I look forward to its publication, which I am told is expected to be published in the spring.
It is vital that workforce planning is closely integrated to the wider planning across health and social care. Health Education England will be merged with NHS England, putting long-term planning and strategy for healthcare staff recruitment and retention at the forefront of the national NHS agenda.
Health and Care Bill: Palliative Care
We must ensure that people receive the most appropriate care personalised to their individual needs as they approach the end of their life.
The NHS Long Term Plan, prepared by the NHS and published in 2019, builds on previous commitments made by the Government to personalise care through informed conversations between healthcare professionals and dying people. Part of this is a commitment to help people to live independently for longer, as well as a promise to give more people more say about the care they receive and where they receive it, particularly towards the end of their lives. I believe empowering people with terminal conditions in this way will better enable them to access palliative care when and where they most need it.
The NHS must meet these commitments, and new measures are being developed to ensure local health and care leaders are meeting the high standards expected of them. There is existing guidance from the National Institute of Health and Care Excellence, which includes specific reference to maintaining comfort in dignity in a person’s last days of life. It is right that clinicians continue to utilise this guidance.
The establishment of the Personalised Care Institute has made training available to help staff identify and support patients and to introduce proactive and personalised care planning for everyone identified as being in their last year of life. Importantly, this enables meaningful conversations to take place and allows staff to help patients and families, address their concerns and to explain the breadth of services available in the local area.
I am encouraged that the Department for Health and Social Care and the NHS proactively engage with the whole sector to understand the issues they face. Most hospices are independent, charitable organisations but do received some funding, mainly from clinical commissioning groups (CCGs), for providing local services. CCGs will have an understanding of future demand and associated funding requirements. There are seven regional Palliative and End of Life Care Strategic Clinical Networks working closely with CCGs and integrated care systems to understand the needs, sustainability and future commissioning of palliative and end of life care services.
Health and Care Bill: Sex-Selective Abortion
Abortion on the grounds of sex alone is illegal and I am glad that the Government guidance for doctors on how to comply with the Act makes this clear. With regard to the Non-Invasive Prenatal Test, this test is never meant to be used to determine the sex of a child, and I share your concerns that this test could be misused to inform sex selective abortion. That is why I am glad that the Government will continue to review the evidence regarding the test.
Health and Care Bill: Private Providers (Integrated Care Boards)
I welcome the intention, through the Health and Care Bill, to develop more integrated care between the NHS, local government, social care providers and other partners to deliver better integration of health and care services on the ground. The reforms proposed in the Health and Care Bill will continue to improve the quality and sustainability of NHS services and outcomes for patients.
Service provision by the independent and voluntary sectors has been, and continues to be, an important and valuable feature of our healthcare system, which I fully support. ICBs are NHS bodies guided by the NHS Constitution and with the values of the NHS at heart. Safeguards are already in place to ensure that the interests of the public and the NHS are always put first. The ICB chair would have the power to veto members of the board and there are robust requirements on ICBs to manage conflicts of interests.
That said, I do appreciate that there are concerns about private sector involvement in ICBs. It is important that people are assured that the work of ICBs will be driven by health outcomes, not by profits.
I welcome therefore that the Government has amended the Health and Care Bill, putting beyond doubt that Integrated Care Boards will not be controlled in any way by the private sector. No one that could potentially undermine the NHS due to their involvement in the private healthcare sector should sit on an ICB. The Government’s amendment [Optional: which I was pleased to support in the Commons] makes clear that no one may be appointed to an ICB who would undermine the independence of the NHS, either as a result of their interests in the private healthcare sector, or otherwise.
It is irresponsible scaremongering to suggest that Integrated Care Boards and Partnerships are being used to support privatisation, or cuts to NHS funding. The NHS will always be free at the point of use, and I believe these reforms will continue to improve the quality of NHS services and outcomes for patients. Ensuring every part of England is covered by an Integrated Care Board and Partnership is a key way of promoting local collaboration.
Primary care commissioners have long had the choice to commission services from a range of primary care providers. I believe it is crucial that local health commissioners have flexibility to commission partnerships, individuals and private and third sector organisations to deliver GP services to meet the specific healthcare needs of their local populations. Alternative Provider Medical Service Contracts (APMS) offer greater flexibility than national standard contracts, allowing commissioners to better meet local need and fill any gaps not covered by core general practice. Private and third sector providers play a vital role in the delivery of local services and must adhere to the same quality and safety standards as any other form of GP contractor.
The Health and Care Bill would extend the oversight that the Secretary of State for Health and Social Care has over the health service in a number of areas. This includes providing direction to NHS England and Improvement and the ability to intervene in health service reconfigurations.
On procurement, the Bill proposes the repeal of a number of clauses in the Health and Social Care Act 2012, including Section 75 which placed requirements on local health bodies to competitively tender for some health care services “where it adds no or limited value”.
The Kings Fund, an independent charity, has said about the reforms: “This Bill will remove cumbersome competition rules and make it simpler for health and care organisations to work together to deliver more joined-up care to the increasing numbers of people who rely on multiple different services.”
November 2021
Dr Liam Fox’s Down Syndrome Bill
Selaine’s response:
I know that with appropriate help and support, most people with Down's syndrome can lead healthy, active and more independent lives, achieving more than ever before. I do recognise, however, that people with Down's syndrome face significant challenges across all stages of life and it is right that the Government considers how to help make sure their specific needs are recognised and considered. That is why I fully support Dr Liam Fox’s Down Syndrome Private Members’ Bill, and I am delighted the Government does too.
The Covid-19 pandemic has further highlighted the need to improve access to services for people with Down's syndrome. The Down Syndrome Bill will require the Secretary of State to publish guidance to public bodies to ensure they are clear on how they should meet the needs of people with Down's syndrome. It will set out best practice across health, education social care and housing, giving practical advice on how the appropriate steps can be taken to meet the needs of those with Down's syndrome when planning, designing and delivering services.
It is especially welcome that the Government will consult widely on the proposed guidance, ensuring the voices of those with Down syndrome, their families and carers are heard, and that the guidance is fit for purpose. This, I believe, is essential.
I would like to take this opportunity to pay tribute to the work of my colleague Dr Liam Fox in bringing forward this important Bill. Whilst I am unfortunately unable to attend the second reading of the Bill,
I look forward to seeing its passage through Parliament and can assure you that the Bill has my full support.
November 2021
Cancer in the Spending Review
Selaine’s response:
I am glad that cancer survival rates have increased year-on-year over the past decade. Investment in research has been vitally important in achieving this and I recognise the important that we continue to invest properly in cancer research so that we can continue to drive up survival rates.
That is why I am pleased that over £882 million in government funding has been spent on cancer research across the UK since 2010. However, I also know that the Covid-19 pandemic has had an impact on cancer research, in particular through reduced access to funding for new projects. Therefore, I welcome the announcement in the Spending Review 2021 that the Government will commit £5 billion over the Spending Review period for health-related research and development, this is an increase of £1.2 billion on previous commitments.
I welcome the announcement that cancer diagnosis is at the heart of the NHS Long Term Plan. Over the ten years to 2023/24, cancer screening and diagnosis will be overhauled with the aim of detecting 75% of cancers in the early stages compared to around 50 per cent today. This will result in 55,000 more people a year living for at least five years following a cancer diagnosis. The Spending Review 2021 provided £2.3 billion to establish 100 new Community Diagnostics Centres to help deliver this.
It is encouraging that the 2021 Spending Review reaffirmed the Government’s commitments to recruiting 50,000 more nurses, providing hundreds of millions of pounds of additional funding over the next four years. I look forward to learning more about the Government’s plans and how this will help to increase the number of cancer nurses in particular. I also warmly welcome the commitment of £2.3 billion in the 2021 Spending Review to transform diagnostic services. This will support the opening of at least 100 community diagnostic centres across England benefitting millions of patients who will be able to access earlier diagnostic tests closer to home.
November 2021
Joint Replacement Surgery
Selaine’s response:
Thanks to the sacrifices of people across the UK, we have been able to protect the NHS from being overwhelmed by Covid-19. The extraordinary efforts of all NHS staff has ensured that the NHS withstood the challenge of the pandemic, treating and caring for millions of people.
Of course, the need to focus on the response to the pandemic meant resources were diverted to tackling the pandemic resulting now in a significant backlog in elective care. In England, 5.7 million people are currently waiting for treatment.
That is why I am glad that the Government is investing an additional £12 billion per year over the next three years in health and social care. I welcome the Government’s commitment to tackling the elective backlog through the biggest catch up programme in the NHS’s history. £2 billion will be spent this year, double the previous commitment, with an additional £8 billion to be spent in the following three years.
This welcome funding could deliver the equivalent of around 9 million more checks, scans and procedures and will mean NHS England can aim to deliver around 30 per cent more elective activity by 2024-25 than before the pandemic. This investment in elective surgery and diagnostic facilities will be vital in allowing those who suffer with arthritis to access the care they need.
November 2021
Funding for Mental Health
Selaine’s response:
While it is hugely welcome that we are on the road to parity of esteem, there is still more to do. That said, I am extremely encouraged by the news that, as part of the five-year funding offer agreed in 2019, mental health services will receive budget growth of £2.3 billion the fastest uplift in funding. This will enable further service expansion and faster access to community and crisis mental health services for both adults and particularly children and young people. I also welcome the Government's commitment of around £2 billion to address waiting times for mental health services, giving more people the mental health support they need, investing in the NHS workforce and helping to ease existing pressures in the NHS caused by Covid-19.
In the 2021 Spending Review, I was encouraged to see a new investment of £150 million in NHS mental health facilities linked to A&E and to enhance patient safety in mental health units. Additionally, around £300 million will be spent to complete the programme of replacing mental health dormitories with single ensuite rooms. The Spending Review also included welcome commitments to supporting ground-breaking innovative research to establish the UK as a life sciences superpower. This includes £95 million for the Office for Life Sciences, which I understand will support the launch of the Prime Minister’s healthcare mission on mental health. I look forward to learning more about this in due course.
I hope these new services help end the stigma surrounding mental health, offering crucial support to people suffering from crisis and those who have suffered in silence for too long.
November 2021
Multiple Sclerosis and Fampridine
Selaine’s response:
With more than 100,000 people across the UK diagnosed with multiple sclerosis, please let me assure you that helping those suffering from this condition to lead as normal lives as possible remains a key commitment of the NHS.
As I understand, diagnosis in the early stages of multiple sclerosis can be difficult, with some of the symptoms often similar to other conditions. I am therefore pleased that the National Institute for Health and Care Excellence (NICE) has produced guidelines to assist clinicians in diagnosing the condition. This guidance also provides clinicians with best practice for treating the many possible symptoms of multiple sclerosis, including mobility problems and fatigue.
I fully appreciate that those suffering from multiple sclerosis may also have specific long-term social care needs. That is why I am glad the Government has prioritised finding a long term social care solution with cross-party support. Better integration between health and social care provision, creating genuinely people-centred coordinated care, is also required, and I look forward to this being explored in forthcoming discussions.
I am encouraged that since 2015, £150.6 million has been spent on Multiple Sclerosis research through the National Institute for Health Research and UK Research and Innovation. This funding demonstrates the commitment both of the Government and of the scientific research community to support people living with MS.
I have been following with interest the experiences of people who have been prescribed Fampridine. In particular, I have read of the experiences of some individuals who took Fampridine during clinical trials, only to see it withdrawn when the trial ended. Improving mobility and, with it, quality of life is something I would expect those drawing up guidelines about the treatment of MS to prioritise. The National Institute for Health and Care Excellence’s (NICE) is updating its guideline on multiple sclerosis, including to take account of new evidence on the effectiveness of Fampridine for treating mobility in people with multiple sclerosis, and this guidance is expected to be published in July 2022. While this is ultimately a matter for NICE, I think it is important that NICE is aware of the strength of feeling about Fampridine and have ensured this is the case.
October 2021
Dementia and Alzheimer's in the Spending Review
Selaine’s response:
I believe that increasing public awareness and understanding of dementia among the wider public is vital to ensure that people are supported to live well with the condition.
Research is crucial to understanding and tackling dementia. Under the Challenge on Dementia 2020 strategy, the Government's commitment to spend over £300 million on dementia research between 2015 and 2020 was met a year early, with £341 million being spent by March 2019. The Government is also supporting the £79 million Accelerating Detection of Disease challenge, a project bringing together the NHS, industry and leading charities to support research into the early diagnosis of disease, including dementia.
I know that the Government remains committed to research, to combat dementia, and will shortly lay out plans for supporting people with dementia in England up to 2025. I look forward to seeing these plans and funding commitments at the next Spending Review. I will work with my colleagues in the Department of Health and Social Care to ensure that the manifesto commitment to double research funding to over £160 million each year by 2030 is delivered as swiftly as possible.
I have spoken with colleagues at HM Treasury about suggestions from some North Devon constituents for the Spending Review taking place this year. While I am not in a position to pre-empt the conclusions of the review, I am assured by my colleagues that they are aware of the points raised. The conclusions will be announced to Parliament alongside the Autumn Budget on 27 October.
Endometriosis and Polycystic Ovary Syndrome
Selaine’s response:
Endometriosis and polycystic ovary syndrome (PCOS) are common long-term conditions that can have a significant impact on a woman’s life, and I am aware of and sympathise with the hardships faced by women who experience severe symptoms. I believe it is important to raise awareness of the impact on women worldwide.
To provide support, all obstetricians and gynaecologists have been trained in the diagnosis and treatment of these conditions; it is a core part of their training. The NHS has published clinical guidelines on the management of endometriosis, and PCOS, to assist doctors. While there is currently no cure, there are several options for treatment and ways that individuals can alter their lifestyle to improve symptoms. NHS England has also developed units for severe endometriosis, with the expectation that all units provide women with severe endometriosis with care which meets the needs of each individual woman. I believe it is essential that care of this kind is specialised to a woman’s unique needs, and I know that Ministers want to empower people to shape and manage their own health and care and make meaningful choices.
The Government launched a consultation to help inform the priorities, content and actions of England’s first Women’s Health Strategy, with questions on gynaecological conditions such as endometriosis. I am told that analysis of the evidence gathered is underway with a view to publishing the strategy later this year. This is a most welcome development and I look forward to learning more about these plans.
I welcome the work of Endometriosis UK and Verity, the UK PCOS Charity, to raise awareness of these conditions, as well as providing sufferers with further information and access to clinical trials and the latest research. Medical Research is funded through the National Institute for Health Research (NIHR) and UK Research and Innovation (UKRI). In the last five financial years, I am encouraged to learn that the NIHR and UKRI have awarded £8.52 million for research into endometriosis and £6.60 million for research into PCOS. This includes a wide range of projects, from basic science through to applied health research into diagnosis, treatment and service delivery. It is important that women with these conditions play a vital role in this research, and I am glad to learn that this is already the case.
While I am unable to attend the upcoming Westminster Hall Debate myself, I will ensure that ministers are aware of the points raised in the campaign emails sent to me.
October 2021
Parkinson’s Related Dementia
Selaine’s response:
The UK Dementia Research Institute (UK DRI), launched in 2017, is the single biggest investment the UK has ever made in dementia thanks to £290 million from founding funders the Medical Research Council (MRC), Alzheimer’s Society and Alzheimer’s Research UK. The UK DRI is leading the UK’s dementia research efforts and tackling the huge challenge of the condition. The Institute will transform treatment and care for people with dementia and is leading the way in early diagnosis and uncovering how to prevent dementia.
The Institute carries out research relevant to all dementias, Parkinson’s related dementia. I look forward to reading more about the experiences of those living with Parkinson's dementia in the Parkinson's UK Report, and while I am unable to attend the event, I will consider the points raised carefully.
October 2021
Epilepsy and Medical Cannabis
Selaine’s response:
There is strong scientific evidence that cannabis can harm people’s mental and physical health, and damage communities. However, recent cases have shown the need to look more closely at the use of cannabis-based medicine in treating patients with very specific conditions in exceptional circumstances, which is why the Government decided it was appropriate to review the scheduling of cannabis.
The decision to reschedule these products means that senior clinicians will be able to prescribe the medicines to patients with an exceptional clinical need. Following short term advice issued in September 2018 the ACMD reviewed the rescheduling in November 2020, and I welcome that they recommended that no changes be made, enabling senior clinicians to continue to prescribe these medicines where appropriate.
Moreover, NHS England has published a review which is aimed at assessing the barriers to prescribing cannabis-based medicinal products where it is safe and clinically appropriate to do so. My ministerial colleagues have also been clear that given the nature of the medicine, it should only be prescribed by specialist doctors and on a case-by-case basis. I believe these controls are necessary to develop clinical expertise and an evidence base for this treatment’s effectiveness.
The National Institute for Health and Care Excellence (NICE) has also developed updated clinical guidance on prescribing cannabis-based products for medicinal use, including for the management of chronic pain. It is crucial that this country keeps in step with the latest scientific evidence, so that patients and their families have access to the most appropriate course of medical treatment. Following difficulties in obtaining prescriptions, I am pleased that NICE has recently published a clarification of this guidance. While this does not represent a change in the law, NICE hopes that it will make prescribing medicinal cannabis clearer and simpler for specialists and therefore easier for patients.
The decision whether to prescribe an individual with medicinal cannabis is therefore not a political or financial decision, but a decision by a medical expert, who will have considered whether it is the most effective treatment based on an individual’s particular condition.
Unfortunately, I will be unable to attend the End Our Pain Campaign’s parliamentary ‘drop in’ event on Tuesday 2 November due to a busy diary, but please be assured I will continue to closely monitor the roll-out of medicinal cannabis.
April 2021
Dementia Research
Selaine’s response:
Having attended an Alzheimer's Research UK event in Westminster and recently visited the Alzheimer's Society stand at the Conservative Party Conference, I am aware of the issues the charities are currently calling for. I hope that increasing public awareness and understanding of dementia among the wider public will ensure that people are supported to live well with the condition.
Research is crucial to understanding and tackling dementia. Under the Challenge on Dementia 2020 strategy, the Government's commitment to spend over £300 million on dementia research between 2015 and 2020 was met a year early, with £341 million being spent by March 2019. The Government is also supporting the £79 million Accelerating Detection of Disease challenge, a project bringing together the NHS, industry and leading charities to support research into the early diagnosis of disease, including dementia.
I know that the Government remains committed to research to combat dementia and will shortly lay out plans for supporting people with dementia in England up to 2025 and I look forward to seeing these plans and funding commitments at the next Spending Review. I will work with my colleagues in the Department of Health and Social Care to ensure that the manifesto commitment to double research funding to over £160 million each year by 2030 is delivered as swiftly as is possible.
I am proud to support a Government that is committed to taking the difficult decisions and tackling these problems head on, creating a sustainable adult care system that is fit for the future. An extra £36 billion will be invested in the health and care system over the next three years, including £5.4 billion in adult social care, to ensure it has the resources it needs to recover from the pandemic. Further, the Government announced a landmark £33.9 billion for the NHS by 2023/24 to secure the long term future of our NHS.
October 2021
Diabetes
Selaine’s response:
Diabetes is a leading cause of premature mortality, doubling an individual's risk of cardiovascular disease. With over 22,000 additional deaths each year, it costs over £10 billion every year to manage. It is right, therefore, that diabetes features prominently in the NHS Long Term Plan (LTP).
While Type 1 diabetes cannot be prevented and is not linked to lifestyle, Type 2 diabetes is largely preventable through lifestyle changes. That is why I am delighted that prevention is at the heart of the NHS Long Term Plan. One of the key commitments in the LTP is to double, to 200,000 people per year by 2024, the scale of the NHS Diabetes Prevention Programme which supports those identified as high risk of type 2 diabetes to reduce their risk.
To date NHS England has invested approximately £120 million of transformation funding into local services to target variation and improve performance in the treatment and care of people living with diabetes since 2017/18. This is focused on improving attendance at structured education to increase understanding, improving achievement of NICE targets and reducing variation across the country, reducing amputations through improved provision of multidisciplinary footcare teams, improving timelines of referrals from primary care for patients with diabetic food disease, and reducing lengths of stay for diabetic inpatients through specialist nursing services.
I absolutely agree that technology could, and should, provide vital support to people managing diabetes and I know that new treatments and technologies are being created all the time. I welcome the DHSC Research and Development Budget for 2021 of £1.3 billion, which underlines the commitment to ensure that the best possible treatments and technologies are available through the NHS at the earliest opportunity.
I hope this reassures you about the commitment to tackling diabetes as well as supporting those living with it to lead healthier lives.
October 2021
Coronavirus: Vaccine and Children
Selaine’s response:
As the Chief Medical Officer has said, the Covid-19 Delta variant is highly infectious and very common, so the great majority of the unvaccinated will catch Covid -19. The likelihood of children becoming severely ill if they catch Covid -19 is thankfully very low, but there is still some risk. I am glad, therefore, that time has been taken to assess this decision carefully and thoroughly.
Earlier this year, the Medicines and Healthcare products Regulatory Agency (MHRA) approved the Covid -19 vaccines supplied by Pfizer and Moderna for 12 to 17 year-olds. It confirmed that both vaccines are safe and effective for this age group. The MHRA is one of the best medical regulators in the world and I can reassure you that authorisation would not be approved unless the expected standards of safety, quality and effectiveness have been met.
While the Joint Committee on Vaccination and Immunisation (JCVI) assessed that the health benefits from vaccination are marginally greater than the potential known harms, the margin of benefit was considered too small to support universal vaccination on this basis alone. That is why additional advice was sought and the UK’s Chief Medical Officers considered the matter from a broader perspective.
In their view, the likely advantages of reducing educational disruption, and the consequent reduction in public health harm, including mental health, from that disruption, on balance provide sufficient benefit in addition to those identified by the JCVI. The CMOs therefore recommend extending the offer of universal vaccination, with a first dose of Pfizer, to all 12 to 15 year olds and the Government has accepted this advice.
I understand that vaccination will be delivered in schools, supported by GPs and community pharmacies. Parental, guardian or carer consent will be sought prior to vaccination, in line with existing programmes. It is important that children can understand the risks and benefits of vaccination for themselves, so it is welcome that information will be provided in a way that is accessible to children and young people as well as their parents.
At every point in the vaccination programme, decisions have been guided by the best clinical advice and I know that this decision is no different. I hope all those aged 12 to 15 will accept this offer of vaccination.
September 2021
Health and Disability Green Paper
Selaine’s response:
I am delighted to see the publication of the Health and Disability Green Paper and the opening of the consultation into shaping future support for disabled people. I would encourage anyone with an interest in this important subject to contribute their views before 11th October via:
https://getinvolved.dwp.gov.uk/05-policy-group/health-and-disability-green-paper/
The Green Paper considers how to improve the DWP’s current services so they are better and easier to use, explore how extra support can help people navigate the system as well as what can be done to better support disabled people into employment. I welcome the wide range of measures discussed in the Green Paper as part of this three-pronged focus, for example, exploring how to improve the information on GOV.UK in order to help people access the relevant benefits online.
I know that DWP has run workshops across the country where local disability organisations and disabled people have shared their experiences and priorities for future change. Additionally, I welcome the publication of the National Strategy for Disabled People, which focuses on issues that disabled people say affect them the most across all aspects of daily life.
The Health and Disability Green Paper is an important step towards improving the way Government supports disabled people and people with health conditions. It focuses on issues that disabled people and people with health conditions have said they would like to see improved and reflects the extensive engagement undertaken before publication.
My colleagues at the DWP recognise that it is essential that any changes made to the health and disability benefits system are shaped by disabled people and their representatives. This is why the Department hosted a series of engagement events across the country, to hear about disabled people’s experiences of DWP services and priorities for future changes. This engagement is continuing through the consultation to ensure that disabled people and people with health conditions help inform potential improvements that we can make.
The consultation closes on 11 October. If you would like to respond you can do so here:
https://getinvolved.dwp.gov.uk/05-policy-group/health-and-disability-green-paper/
Consultation responses will inform a White Paper, which is due to be published next year.
September 2021
Private Providers (Integrated Care Boards)
Selaine’s response:
I welcome the intention, through the Health and Care Bill, to develop more integrated care between the NHS, local government, social care providers and other partners to deliver better integration of health and care services on the ground. The reforms proposed in the Bill will continue to improve the quality and sustainability of NHS services and outcomes for patients.
Service provision by the independent and voluntary sectors has been, and continues to be, an important and valuable feature of our healthcare system, which I fully support. Safeguards are already in place to ensure that the interests of the public and the NHS are always put first. The Integrated Care Board (ICB) chair would have the power to veto members of the board and there are robust requirements on ICBs to manage conflicts of interests.
That said, I do appreciate that there are concerns about private sector involvement in ICBs. It is important that people are assured that the work of ICBs will be driven by health outcomes, not by profits.
I know that the Bill does not allow private sector providers to influence, or to make, decisions on spending, but it is welcome that the Government has committed to putting that beyond doubt. They will bring forward an amendment at the next stage of the Bill’s passage through Parliament to protect the independence of ICBs by preventing individuals with significant interests in private healthcare from sitting on them. I know that ministerial colleagues will be working to ensure that any amendment is appropriately worded and does not have any unintended consequences. I look forward to seeing their proposed amendment in due course and can assure you that I will scrutinise its contents closely.
September 2021
Dementia
Selaine’s response:
I believe that increasing public awareness and understanding of dementia among the wider public is vital to ensure that people are supported to live well with the condition, and I am encouraged that there are over three million Dementia Friends, including myself, a national support network run by the Alzheimer’s Society which helps dementia sufferers to lead lives that are active, creative and meaningful.
Research is crucial to understanding and tackling dementia. In 2017, the Government launched the UK Dementia Research Institute, in partnership with the Alzheimer's Society and Alzheimer's Research UK, with £290 million funding, the single biggest investment ever made in the UK in this field. Under the Challenge on Dementia 2020 strategy, the Government's commitment to spend over £300 million on dementia research between 2015 and 2020 was met a year early, with £341 million being spent by March 2019 through the Department of Business, Energy and Industrial Strategy, and the Department of Health and Social Care. The Government is also supporting the £79 million Accelerating Detection of Disease challenge, a project bringing together the NHS, industry and leading charities to support research into the early diagnosis of disease, including dementia.
By the end of 2020, all relevant staff were scheduled to have received appropriate dementia training, including training relevant staff to be able to signpost interested individuals towards research via the Join Dementia Research Service. I understand that good progress has been made towards this goal, and more options are currently being explored to increase take-up of more advanced training among those who need it.
Last year the Prime Minister announced the Government’s intention to provide the NHS with an additional £33.9 billion by 2023/24; this is the largest, longest funding settlement in the history of the NHS. This landmark settlement investment will secure the long term future of our NHS and demonstrates the Government’s commitment to fund our NHS and public services properly. As part of this, there is a commitment to improving detection, with more targeted screening and Rapid Diagnostic Centres, so that in ten years’ time these measures will help 55,000 more people to survive cancer each year, and prevent 100,000 heart attacks, strokes and dementia cases.
I am pleased that Alzheimer Research UK is holding an event on 15 September, and I will be attending.
August 2021
Self-Isolation
Selaine’s response:
We are seeing an increasing number of people being asked to self-isolate as the case number across the country rise. Self-isolation has played a critical role in helping to control the Covid-19 outbreak by denying the virus the human contact that it needs to spread. I know we are all grateful to the many people all across the UK, who have selflessly done their duty and self-isolated, making sacrifices to keep the virus at bay.
It is the responsible thing to do to self-isolate when told to do so and I am disappointed when I hear that some businesses are asking employees to ignore the advice from the NHS.
As part of step 4 of the Government’s Covid-19 roadmap, double vaccinated people will no longer be legally required to self-isolate if they are identified as a close contact of a positive Covid-19 case. The new rules are due to come into effect from 16 August. To ensure young people can make the most of their education as restrictions continue to ease, under 18s will also be exempt from self-isolation if they are a close contact.
I am keen for this to be introduced as soon as possible as this will also help reduce the number of self-isolations that may not be necessary after a negative test.
Young people and double vaccinated individuals, identified as close contacts, will continue to be advised to take a PCR test, to detect the virus and variants of concern. Anyone who tests positive following the PCR test will still be legally required to self-isolate, irrespective of their vaccination status.
The pandemic is far from over, and it is right that we all continue to act with caution. However, we can take hope from the fact that science has shown us the way forward in the form of the vaccine, just as it has done so many times throughout our fight against this virus. I urge everyone to take up the offer of a vaccination as soon as they are able.
The next few weeks will be difficult for many employees and employers, but I urge patience and understanding. I am seeing many businesses and many of the services provided by our councils choosing to continue with some or all the procedures that we have all become accustomed to over the last few months. I welcome and appreciate this, while the legal restrictions may have been removed, we still have a responsibility to act in a safe and reasonable manner, for both ourselves and others. Many businesses are understandably reflecting the caution that the majority of their customers want to see.
Government instruction and in some cases extreme intervention into our daily lives has been necessary in the global emergency, but the recent legal restrictions we have faced must be the exception, not the rule. We all know how the virus transmits and I believe at this time can take responsibility for our actions as we learn to live with this coronavirus moving forward.
July 2021
Maternity Care: Continuity of Carer and Baby Loss
Selaine’s Response:
I believe that every woman and their baby should receive personalised, high quality care. One of the key commitments in the NHS Long Term Plan (LTP) published in January 2019 is to make the NHS one of the safest places in the world to give birth. The Government has set out a range of new measures to deliver its ambition to halve the rates of stillbirths, neonatal deaths and brain injuries that occur during or soon after labour, and maternal deaths by 2025. To help meet this target, I welcome the Government’s announcement that it will recruit 3,000 more midwives.
I firmly agree that the continuity of carer model is extremely important, and is associated with reduced pre-term births, hospital admissions, reduced need for intervention during labour, and an improved experience of care. Local maternity units are rolling out a standard continuity of carer model and the NHS Planning Guidance 2019/20 stated that that they should prioritise women who could be at higher risk. Please be assured that work is ongoing to roll out this model, though that has been slightly more difficult during the 12 months of the Covid-19 pandemic.
While it is welcome that the target to reduce neonatal stillbirth and neonatal mortality rates by 20% by 2020 was met, with almost a 25% reduction reported, more work is being done in this area to further reduce these rates. Losing a baby is devastating, and it is vital we do everything possible to ensure that parents who have previously lost a baby are properly and consistently supported through any future pregnancies. I was unfortunately unable to attend the Westminster Hall debate on “Progress towards the National Ambition to reduce baby loss', I understand that this is close to the hearts of constituents and will ensure I follow this matter closely.
July 2021
Health and Care Bill
Selaine’s response:
The unprecedented threat of the Covid-19 pandemic has reminded us how vital our health and care system is to all of us. I want to assure constituents that the NHS will always be free at the point of use, and any proposed reforms will aim to continue to improve the quality of these services and patient outcomes.
As we build back better from this pandemic, it is right and necessary that our health and care services are at the forefront. The pandemic underlined not only the dedication and skill of those in this sector, but also the necessity of a broader, more integrated health and care system. I welcome the intention to develop more joined up, integrated care between the NHS, Local Government and other partners including the voluntary and community sector, which will be vital in tackling the factors that affect the long-term sustainability of patient services. The Bill will make permanent some of the innovations we have seen as a result of the pandemic. I understand that these proposed reforms will also include proper accountability mechanisms and give patients and the public the confidence that they are receiving the best care from their healthcare system.
The measures set out in the Health and Care Bill deliver on the NHS’s own proposals for reform in its Long Term Plan. I believe these proposals have been developed in consultation with key stakeholders in this sector, and I am encouraged by the preliminary positive feedback received.
In particular, the comments from the Chief Executive of NHS England, who has said that this Bill “will support our health and care services to be more integrated and innovative so the NHS can thrive in the decades to come”, are reassuring.
July 2021
Adult Social Care
Selaine’s response:
I believe we must all receive dignified care in old age, and with an ageing population, this is one of the biggest challenges our country faces, and I stand by the Government’s commitment to ensure that the most vulnerable in society are given the support that they need.
While it is important to note that as of June 2021, 84% of all social care settings were rated good or outstanding by the Care Quality Commission, more needs to be done to tackle this serious challenge, crucially by securing a long term funding solution.
I am delighted that the Prime Minister has spoken of his determination to tackle this, stating in his first speech as Prime Minister that “we will fix the crisis in social care once and for all with a clear plan we have prepared, to give every older person the dignity and security they deserve”.
At the Spending Review in November 2020, local authorities were enabled to access over £1 billion of spending for social care, through £300 million of social care grant, and the ability to levy a 3% adult social care precept. This is in addition to the £1 billion social care grant announced during 2019, and the £3 billion provided to local authorities to address Covid-19 pressures, including in adult social care. I know that this Government is committed to sustainable improvement of the adult social care system.
Money alone will not fix the problem, and reform is needed to encourage high standards across the whole country. It is vital for us to consider ways of better joining up health and care services, and I am encouraged by the use of the Better Care Fund to assist local government and the NHS with the implementation of integrated health and care services.
In the Conservative Manifesto, on which I was proud to stand, we set out our aim to build the same level of consensus on social care that we have already built on the NHS, across political parties, so that an answer can be brought forward that solves the problem, commands the widest possible support, and stands the test of time. I firmly support the renewed commitment in the Queen's Speech to bring forward proposals to reform social care during this Parliament, and eagerly anticipate taking part in a conversation about establishing a care system fit for the 21st century.
July 2021
NHS England Reform
Selaine’s response:
The unprecedented threat of the Covid-19 pandemic reminded us how vital our health and care system is to all of us. I want to assure constituents that the NHS will always be free at the point of use, and any proposed reforms will aim to continue to improve the quality of these services and patient outcomes.
As we build back better from this pandemic, it is right and necessary that our health and care services are at the forefront. The pandemic underlined not only the dedication and skill of those in this sector, but also the necessity of a broader, more integrated health and care system. I welcome the intention to develop more joined up, integrated care between the NHS, Local Government and other partners including the voluntary and community sector, which will be vital in tackling the factors that affect the long-term sustainability of patient services. I understand that these proposed reforms will also include proper accountability mechanisms, and give patients and the public the confidence that they are receiving the best care from their healthcare system.
I believe these proposals have been developed in consultation with key stakeholders in this sector, and I am encouraged by the preliminary positive feedback received. In particular, the comments from Nigel Edwards, the Chief Executive of the health policy think tank the Nuffield Trust, that these proposed reforms would allow GPs, hospitals, community services and social care to “work better and more effectively together” in the longer term are reassuring.
NHS managers have played a vital role throughout this pandemic, and I am pleased that Chris Hopson of NHS providers, which represents NHS managers, agrees with these reforms that will end the “unnecessarily rigid NHS approach to procurement”. It is also welcome that this White Paper enacts the recommendations of the 2019 Kark Review for stronger measures to ensure that NHS senior managers have the right skills, behaviours and competencies. I understand that there are no plans at this stage to statutorily regulate senior NHS managers and leaders, and I will continue to monitor this closely.
More broadly, I am pleased at the Government’s clear commitment to supporting the NHS and our wider healthcare system. The Government will provide the NHS with £33.9 billion in funding by 2023/24, which is the largest, longest funding settlement in the history of the NHS, and is confirmed in law by the NHS Funding Act. In addition, the NHS Long Term Plan commits £4.5 billion in primary and community care to help strengthen local healthcare networks.
July 2021
Coronavirus: Vaccine Boosters (Asthma)
Selaine’s response:
The Joint Committee on Vaccination and Immunisation (JCVI) concluded that only those with more severe forms of asthma are at clinically high risk from Covid-19. This group are defined as adults with asthma who require continuous or repeated use of systemic steroids or with previous exacerbations requiring hospital admission and will have been eligible for vaccination as part of priority group six. An individual with a more severe case of asthma may have been included in the clinically extremely vulnerable group, in which case they will have been eligible as part of priority group four.
To assist GPs in identifying patients eligible for a vaccine in each priority cohort, NHS Digital aligned specifications for the identification of patients via their medical records with GP system suppliers. Asthma sufferers were identified through this system and invited to make an appointment when the vaccination programme reached their priority cohort.
While the programme of first and second doses continues, the Government has confirmed that a booster shot programme will happen in the autumn and steps are being taken to prepare for this. Of course, some logistical matters remain to be resolved, but it is anticipated that the booster programme will be rolled out in a similar way to the current programme albeit with some differences for example to account for the annual flu vaccination programme.
June 2021
Mental Health Support for Young People with Cancer
Selaine’s response:
Improving outcomes for patients diagnosed with cancer remains a key NHS priority. Last December, the Minister for Prevention, Public Health and Primary Care said that "the Government will stop at nothing to make childhood cancer a thing of the past for generations to come", a commitment which I firmly support.
I absolutely believe that we must do all we can to provide appropriate support to those suffering with cancer and their families. NHS Cancer Services for Teenagers and Young Adults must meet a wide range of criteria which not only includes establishing clear care pathways and providing the best medical care, but also assigning a key worker and providing support at every stage. This includes ongoing physical and emotional support during and after treatment is finished.
I know that my colleagues across Parliament, as well as charities and health teams are working to make sure that everything possible is done to ensure children and young people with cancer, as well as their families, have access to appropriate psychological support.
June 2021
Arthritis, Joint Replacement Surgery and the impact of the Pandemic
Selaine’s response:
I would like to first commend Versus Arthritis for their work to support people suffering with arthritis and to raise awareness of the condition.
I am grateful to everyone who has worked so hard to stay at home throughout the pandemic. Their efforts have undoubtedly saved lives and enabled our NHS to provide urgent treatment like cancer and emergency care. However, I understand that 4.7 million people in England are now waiting for care, with around 380,000 of those having been waiting more than a year, in addition to people who have not contacted their GP when, in ordinary times, they would have reached out for help. I believe that we must act urgently to tackle this problem.
As a result, I welcome that the Government is already working with the NHS to accelerate service recovery. In March 2021, an additional £7 billion of funding was announced for healthcare services, including £1 billion to target backlogs in elective services. As part of the commitment to the recovery of non-urgent services and to address elective backlogs, £325 million has been provided for new investment in diagnostics equipment to improve clinical outcomes.
I know that staff throughout the NHS are working extremely hard to tackle the backlog, indeed in January and February 2021 NHS staff completed almost 2 million operations and other elective care while also providing treatment to 140,000 Covid-19 patients in England. However, I agree that there is more work to be done in this area over the coming months.
June 2021
Children and Young People's Mental Health
Selaine’s response:
It is incredibly important to protect and support the health of children and young people in our society. In recent years we have made huge progress in understanding mental health issues, and I support efforts to transform children and young people’s mental health for the better. Approximately 10% of 5 to 16 year olds have a clinically diagnosable mental health problem, and since 2015, an additional £1.4 billion has been invested to transform children and young people’s mental health services.
The Children and Young People’s Mental Health Green Paper sets out ambitious proposals to improve mental health services for children and young people, together with over £300 million of funding. This will incentivise and support schools and colleges to train designated leaders for their pupils’ mental health, and introduce new mental health teams, both of which will ease pressure on NHS mental health services.
The NHS Long Term Plan makes a commitment to offering children and young people the best start in life. As part of this, there is an additional commitment to deliver on the promises made in the ‘Five Year Forward View for Mental Health’ so that 70,000 more children and young people will access treatment each year by April 2021. Moreover, by 2023/2024 at least an additional 345,000 children and young people aged 0-25 will be able to access support via NHS funded mental health services and school or college-based Mental Health Support Teams. In particular, I welcome the Secretary of State's announcement that £79 million from the additional £500 million for mental health announced at the 2021 Spending Review will be allocated to accelerate the commitment to expand these services.
Early intervention is absolutely vital in the fight against eating disorders and everyone with an eating disorder must have access to timely treatment. That is why I am glad that an ambitious new access standard has been introduced, aiming for 95% of children (up to 19 years old) with eating disorders to receive treatment within a week for urgent cases and four weeks for routine cases by the end of 2020. While in view of the coronavirus pandemic I know that this has been a particularly challenging year, and I share my constituent's disappointment that this target was not met, I know that NHS staff have been working extremely hard to refer people as quickly as possible. I am certain that services will continue to improve, particularly as NHS services return to normal following the disruption of the past year.
June 2021
Abortion ('DIY Abortions')
Selaine’s response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings around this matter. It is for this reason that, as with other matters of conscience, the Government adopts a neutral stance on abortion, allowing Conservative MPs to vote freely according to their moral, ethical, or religious beliefs. This is a convention which I support wholeheartedly.
Abortion care is an essential part of care for women, and safeguarding measures are still in place as part of care during the pandemic. The Royal College of Obstetricians and Gynaecologists has offered guidance on this issue which can be found here:
Guidelines have been issued which enable women to take both Mifepristone and Misoprostol at home for the duration of the outbreak, so that they do not have to visit a medical practice and risk exposure to the virus, and to enable doctors to prescribe medicines from home via telephone or video consultations without consulting a second practitioner, so that abortion care can be provided even in the case of staff shortages. I have been assured this alteration will last only as long as the temporary provisions enacted by the Coronavirus Act 2020 to protect women seeking care endure. The medicines must still be instigated prior to nine weeks and six days into the pregnancy. I am aware of data that indicates an increase in the number of abortions carried out in April 2020 by comparison with April 2019; I am also aware that the same dataset shows lower abortion rates during May and June 2020 compared with the same months in 2019.
The pandemic has had an impact on many aspects of daily life, the full picture of which may not be clear for some time to come. I will, of course, continue to monitor this sensitive issue.
A consultation was held to explore whether these temporary changes should be enacted long term, the results of which are currently being analysed. You can find more information on that here:
https://www.gov.uk/government/consultations/home-use-of-both-pills-for-early-medical-abortion
I understand that making a decision regarding abortion care can be an extremely difficult one, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all of their options, with medical professionals offering impartial advice. I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion care including all options available to them.
June 2021
Animal Research
Selaine’s response:
Animal research still plays a role in providing vital safety information for potential new medicines. It is worth remembering that, as a result of findings from animal studies, a large number of potential new drugs never get as far as being tested in humans. Some aspects of the toxicological assessment of new medicines cannot be adequately assessed in humans, and animal data will be the only kind available.
Without animal testing it is highly likely that a large number of potentially dangerous new medicines would be tested in healthy volunteers and patients in clinical trials, and I know ministers believe that this would be quite unacceptable. However, animals are only used when there are no suitable alternatives, and by encouraging new cutting-edge approaches to science we will ensure that standards of animal welfare are improved. I am absolutely opposed to animal tests where alternative approaches could be used.
I fully support all steps to establish new methods and to support the life sciences and research industry. Since 2017, the Government has invested around £1 billion through two Life Sciences Sector Deals, helping to generate significant levels of industry investment in the UK. I am committed to making the UK the leading global hub for life sciences. The Life Sciences Investment Programme (LSIP) aims to unlock the potential of the UK’s best health and life science innovations, allowing companies to grow in the UK. This investment programme consists of up to £600 million of joint Government and industry investment.
It is important to remember that existing scientific research methods ensure that by the time medicines reach clinical trial, risks are significantly reduced.
June 2021
Inpatient Units
Selaine's response:
I absolutely believe that patient safety and care for those with autism and learning disabilities should be to the highest standard and I am deeply concerned at the abuse that patients in Winterbourne and other hospitals faced.
Children, young people and adults with a learning disability, autism, or both, with the most complex needs, have the same rights to live fulfilling lives. Since 2015, the number of people in inpatient care has reduced by almost a fifth, which is welcome progress.
The NHS Long Term Plan sets out key changes to inpatient units for those with learning disabilities and autism. This includes a commitment to reducing the number of admissions and decreasing the amount of time spent in these units.
However, I do appreciate the need to do all we can to support the prevention of inpatient admission and so it is welcome that the Long Term Plan includes increased investment in intensive, crisis and forensic community support. This will enable more people to receive personalised care in the community, closer to home, and reduce preventable admissions to inpatient services. Local providers will also be able to take control of budgets to reduce avoidable admissions, enable shorter lengths of stay and end out of area placements.
I firmly support the four principles set out in the Government’s proposed changes to the Mental Health Act as an important measure for protecting patients, service users, and their loved ones. I understand that the Government is currently reviewing feedback from the consultation on reforming the Mental Health Act, which included consideration of the introduction of new duties on commissioners to ensure the adequate supply of community services for people with a learning disability and autistic people.
I will of course continue to monitor this issue carefully and contact ministerial colleagues to ensure that these changes work for patients, families and carers.
June 2021
Health and Disability Green Paper
Selaine’s response:
I appreciate that there is frustration at the delay to the Health and Disability Green Paper, but it is my understanding that, given the necessary focus on the departmental response to Covid-19, the Department for Work and Pensions (DWP) are working to a longer timescale than previously anticipated. The Minister for Disabled People is continuing to engage with disabled people and their representatives and is committed to publishing the formal consultation document in the coming months.
The Green Paper will consider how to improve the DWP’s current services so they are better and easier to use, explore how extra support can help people navigate the system as well as what can be done to better support disabled people into employment.
The DWP has run workshops across the country where local disability organisations and disabled people have shared their experiences and priorities for future change. Additionally, the Government plans to publish a National Strategy for Disabled People, which will focus on issues that disabled people say affect them the most across all aspects of daily life.
June 2021
HIV Action Plan
Selaine’s response:
Please allow me to assure you that every effort is being made to fight discrimination surrounding HIV and AIDS, and to ensure that those affected can access the necessary treatments available to them. I know that treatment for HIV has continued throughout the Covid-19 crisis.
While I welcome the news that new HIV diagnoses across the UK fell by 15% between 2017 and 2018, more remains to be done. That is why I support the Government’s commitment to stopping new HIV infections by 2030, through a National HIV and Sexual Health Promotion programme. Additionally, following the success of the NHS England funded three-year impact trial of pre-exposure prophylaxis (PrEP), for HIV prevention, I was delighted to learn that PrEP is becoming routinely available across England since March 2020, as part of the government's aim to end HIV transmission by 2030.
The funding from the Department of Health and Social Care will ensure anyone who is at a high risk of contracting HIV will receive PrEP from their local sexual health clinic to reduce their risk of getting the virus. NHS England will cover the costs of the drug and local authorities will be supported with £16 million funding to deliver services.
I welcome the Government’s continued work with charities such as the Terence Higgins Trust and the World AIDS Day initiative, in order to raise awareness of HIV and reach groups with the highest rates of the infection.
June 2021
Crohn's and Colitis
Selaine's response:
I know Crohn's, Colitis and other Inflammatory Bowel Diseases (IBDs) can have a deep and lasting impact on quality of life, and it is essential that those living with this condition are aware of the specialist services available from the NHS.
IBD affects over 300,000 people in the UK, but there is relatively low public awareness, which poses difficulties for sufferers. I am pleased to see that NHS Choices, and charitable organisations such as Crohn’s and Colitis UK, work tirelessly to improve public awareness, and provide useful information on the symptoms, diagnosis and treatment.
The National Institute for Health and Care Excellence has published guidance for the management of IBD, which states that sufferers should receive treatment from a local Multidisciplinary Team, comprising of a range of experts, from dieticians to specialist clinical nurses. I am also glad that the guidance states that patients considering or undergoing surgery, should receive information about their treatment from a specialist.
The Department of Health funds research through the National Institute for Health Research (NIHR). NIHR welcomes funding applications for research into any aspect of human health, including Crohn’s disease, IBS, and Ulcerative Colitis.
I appreciate that long-term conditions like IBD can affect a person’s ability to work. Patients may be entitled to reclaim hospital travel costs through the Healthcare Travel Costs Scheme, available on the NHS Choices website www.nhs.uk and those too ill to work may receive benefits. Information about financial assistance for sufferers of disabling long-term conditions can be found here: www.gov.uk/financial-help-disabled.
I have been most interested to learn more about the impacts of IBD through IBD UK's report The Hidden Cost and a Vision for Change. I was pleased to learn that 72% of respondents rated the quality of their care as excellent, very good or good. I would certainly be happy to work to raise awareness of the symptoms among the public and among healthcare professionals to assist with more swift diagnosis, and to learn more about the other recommendations in the report.
While I understand that progress on the inflammatory bowel disease RightCare scenario has been delayed due to Covid-19 pressures, a working draft has been reviewed and commented on by NHS England and NHS Improvement’s working group and by Crohn’s and Colitis UK.
NHS England and NHS Improvement are in the process of updating the original working draft based on these comments. It is anticipated that a revised version will be ready to be share with IBD UK and their partner organisations for consultation in May, and I look forward to having the opportunity to review this document at the earliest opportunity.
May 2021
Catch up with Cancer Campaign
Selaine’s response:
I was delighted when it was announced that NHS services could begin restarting from April, starting with the most urgent, like cancer care and mental health support. The NHS is open for business, even during this time of additional restrictions, and anyone who needs care and treatment should continue to access it as and when they need it, especially when delays could impose both an immediate and a long term risk to health.
Cancer is a priority for the Government and survival rates are at a record high. Since 2010 rates of survival from cancer have increased year-on-year. Around 7,000 people are alive today who would not have been had mortality rates stayed the same as then. I agree that we need to keep working on this, which is why I welcome the Government's stated aim to see three quarters of all cancers detected at an early stage by 2028 (currently just over half are detected at an early stage). The plan will overhaul screening programmes, provide new investment in state-of-the-art technology to transform the process of diagnosis, and boost research and innovation. This is part of the NHS Long Term Plan (LTP), published in January 2019, and forms part of how the Government will achieve its ambition to see 55,000 more people surviving cancer for five years in England each year from 2028.
I will continue to support the Government and the NHS to deliver on this, in spite of the ongoing coronavirus pandemic. In particular, I welcome that the Government has already announced £3 billion funding to support the NHS recovery from Covid-19, to help to ease existing pressures and enable hospitals to carry out extra checks, scans, and other operations or procedures. This will help to ensure that cancer patients are able to access the care that they need as safely and quickly as possible. This was reiterated as part of the Spring Budget 2021, and I firmly support the Government's ongoing commitment to the NHS and the vital service it provides, during normal times as well as the pandemic.
One of the measures outlined in the LTP is safer and more precise treatment, including advanced radiotherapy techniques and immunotherapies to continue to support improvements in survival rates. This will be supported by a £130 million upgrade of radiotherapy machines across England, as well as commissioning the NHS new state-of-the-art Proton Beam facilities in London and Manchester. In addition, the LTP commits to reforms to the specialised commissioning payments for radiotherapy hypofractionation to support further equipment upgrades. Faster, smarter and effective radiotherapy, supported by greater networking of specialised expertise, will mean more patients are offered curative treatment, with fewer side effects and shorter treatment times. Starting with ovarian cancer, the NHS will ensure greater access to specialist expertise and knowledge in the treatment of cancers where there are fewer or more risky treatment options.
I fully intend to attend the virtual Cancer Summit on Wednesday 26th May, to ensure I am aware of the latest updates and information.
May 2021
British Sign Language
Selaine’s response:
Deafness or being hard of hearing should not be a barrier to participating in society and I understand the desire to see British Sign Language (BSL) recognised as an official language of the UK. If I were successful in the Private Members Bill ballot, I would instigate a survey of the constituency to ascertain which bill would be the best one to progress to fully represent what is important for the constituents of North Devon. I am not averse to this bill, but I would want to see what else there is that needs addressing before committing to any particular bill.
It is clear to me that the Government and the public sector should lead by example in ensuring that important communication is accessible to all. I am, therefore, glad that public health information has been available in many alternative formats including BSL during the Covid-19 outbreak. Covid-19 press briefings with BSL have been available on the Downing Street social media channel and the BBC News channel has provided live BSL interpretation for the briefings.
BSL, more broadly, may also be offered in schools as part of the school curriculum. I understand that the Department for Education is working to develop draft content for a potential GCSE in BSL and that a consultation on the content is due to published this year.
May 2021
Dementia
Selaine’s response:
Research is crucial to understanding and tackling dementia. In 2017, the Government launched the UK Dementia Research Institute, in partnership with the Alzheimer's Society and Alzheimer's Research UK, with £290m of funding, making it the single biggest investment ever made in the UK in this field.
Under the Challenge on Dementia 2020 strategy, the Government's commitment to spend over £300m on dementia research between 2015 and 2020 was met a year early, with £341m being spent by March 2019 through the Department of Business, Energy and Industrial Strategy, and the Department of Health and Social Care. The Government is also supporting the £79m Accelerating Detection of Disease challenge, a project bringing together the NHS, industry and leading charities to support research into the early diagnosis of disease, including dementia.
By the end of 2020, all relevant staff were scheduled to have received appropriate dementia training, including training relevant staff to be able to signpost interested individuals towards research via the Join Dementia Research Service. I understand that good progress has been made against this goal, and more options are currently being explored to increase take-up of more advanced training among those who need it.
The Prime Minister recently announced the Government’s intention to provide the NHS with an additional £33.9 billion by 2023/24; this is the largest, longest funding settlement in the history of the NHS. This landmark settlement investment to help secure the long-term future of our NHS is extremely welcome, and I hope you agree it demonstrates the Government’s commitment to properly funding our NHS and public services. As part of this, there is a commitment to improving detection, with more targeted screening and Rapid Diagnostic Centres, so that in 10 years time these measures will help achieve 55,000 more people surviving cancer each year, and 100,000 heart attacks, strokes and dementia cases being prevented.
The Government is integrating and improving health and social care to protect people at every stage of their lives. In the manifesto on which I was proud to stand it was made clear that we must build the same level of consensus on social care that we have already built on the NHS, across political parties, so that an answer can be brought forward that solves the problem, commands the widest possible support, and stands the test of time. I stand by this commitment, and urge my colleagues and constituents of all political beliefs to take part in a conversation about establishing a care system fit for the 21st century.
I know that the Government remains strongly committed to research to combat dementia, and will shortly lay out plans for supporting people with dementia in England up to 2025. Sadly, I understand that the mobilisation of the health research system against Covid-19 will have an impact on the speed with which the Dementia Moonshot plans can be implemented. However, I will work with my colleagues in the Department of Health and Social Care to ensure that the manifesto commitment to double research funding to over £160m each year by 2030 is delivered as swiftly as is possible.
I believe increasing public awareness and understanding of dementia among the wider public is vital to ensure that people are supported to live well with the condition and I am encouraged that there are over 3 million Dementia Friends.
April 2021
Disabled Children's Partnership Campaign
Selaine’s response:
I can only imagine the additional challenges for disabled children and their families during the pandemic, and I welcome the work of the Disabled Children's Partnership in highlighting this issue through the Left in Lockdown campaign. I am determined that disabled children and their families in North Devon should receive the support they need to lead fulfilling lives and be part of the community. I wholly support the excellent work this campaign is doing to highlight the reality of the challenges disabled children, young people and their families face in living a life many of us take for granted.
As part of the Covid-19 mental health and wellbeing recovery action plan, the Government announced £79 million of funding to improve access to mental health services for children and young people, including disabled children. This includes additional funding for Mental Health Support Teams in schools and colleges. Funding is also provided for respite care.
Further, supporting children and young people with special educational needs and disabilities (SEND) and their families is a priority for this government, and their educational, physical and mental wellbeing remains central to our cross-government response to the Covid-19 outbreak. That is why education settings have remained open for children and young people with an education, health and care plan throughout periods of national lockdown.
The return to school for all pupils was prioritised due to the significant and proven impact caused by being out of school, including on wellbeing. The support schools provide to their pupils as they return to face-to-face education should include time devoted to supporting wellbeing, which will play a fundamental part in supporting children and young people’s mental health and wellbeing recovery. The expectations for schools in this regard are set out clearly in the main Department for Education guidance to schools, which also signposts further support, available here:
https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak
I am encouraged by the commitment to improve opportunities and life chances for all children and young people, and I know that health and care services play an integral part in achieving this.
April 2021
NHS and Centene
Selaine’s response:
I understand that a number of constituents have concerns about Centene's involvement in GP surgeries. I would like to reassure those constituents that patient care will not be affected, and all services will remain free at the point of delivery. As with all GP services, those for which Centene is responsible will continue to be regulated and inspected by the Care Quality Commission. The Clinical Commissioning Groups where this has happened have followed the appropriate and robust processes prior to transfer of responsibility to Centene. The NHS has always involved a mixture of public and private provision, and it is absolutely not for sale to private providers.
March 2021
COVID-19 Recovery Plan for Children with SEND
Selaine’s response:
I know that the pandemic has presented many difficulties and challenges for children and young people with special educational needs and disability (SEND), so I am pleased that supporting them is a priority for the Government. I welcome that the specific needs of children and young people with SEND are considered as a priority for education recovery work, and that Sir Kevan Collins has been appointed as Education Recovery Commissioner to deliver this programme.
To help support families of children with SEND, £40.8 million has been provided for the Family Fund during 2020-21, including £13.5 million to respond to the impact of the outbreak of coronavirus. This funding has helped to support over 80,000 low-income families raising children with disabilities or serious illnesses. Separately, over £42 million has been allocated to extend contracts and grants which enable schools, colleges, families, and local authorities to support thousands of children with SEND.
High Needs Funding has been boosted by £780 million throughout 2020-21, and that a further £730 million will be provided for 2021-22. A consultation was recently held on a number of small technical changes to the High Needs National Funding Formula (NFF) for the 2022-23 financial year, and I welcome that the consultation represents the first stage of a longer-term review of the High Needs NFF which will consider how the distribution of funding can be improved to achieve the highest quality support for the most vulnerable children and young people.
Helping all pupils to catch up on learning lost as a result of the pandemic is of paramount importance, and it is welcome that a £1.7 billion recovery package has been created. This includes £83 million to expand the National Tutoring Programme (NTP) and I am pleased that, of the 33 NTP providers, 26 have specific expertise in supporting children with special educational needs. Providers of the 16-19 Tuition Fund, which received a £102 million extension, have also been asked to have regard for the needs of pupils with SEND when making prioritisations for small group tuition.
March 2021
Telemedical Abortion
Selaine’s response:
I completely understand what an incredibly emotive issue this is, and I appreciate the strength of feelings on all sides. Abortion care is an essential part of care for women, and I would like to make the reassurance that safeguarding measures are still in place.
The Royal College of Obstetricians and Gynaecologists has offered guidance on this issue which can be found here: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-abortion/information-for-women/
Guidelines have been issued which enable women to take both Mifepristone and Misoprostol at home for the duration of the pandemic, so that they do not have to visit a medical practice and risk exposure to the virus, and to enable doctors to prescribe medicines from home via telephone or video consultations without consulting a second practitioner, so that abortion care can be provided even in the case of staff shortages.
I have been assured this alteration will last only as long as the temporary provisions enacted by the Coronavirus Act 2020, to protect women seeking care endure, and the medicines must still be instigated prior to nine weeks and six days into the pregnancy. I understand that a consultation has been announced to explore whether these temporary changes should be enacted long term. You can find more information on that here: https://www.gov.uk/government/consultations/home-use-of-both-pills-for-early-medical-abortion
Making a decision regarding abortion care can be an extremely difficult time, and I believe that we must do all we can to support women to make an informed decision, taking into consideration all their options, with medical professionals offering impartial advice. I will continue to do all I can to ensure plenty of information is available to women making enquiries relating to abortion care including all options available to them.
March 2021
Motor Neurone Disease (MND)
Selaine’s response:
With early diagnosis key to treating the symptoms of MND, I am glad that the National Institute for Health and Care Excellence (NICE) has published new guidelines for clinicians on the assessment and management of MND. These set out the signs and symptoms of the disease, and recommend that patients suspected of having MND should be referred without delay. The Royal College of GPs and the MND Association have also worked together to produce a Red Flag Tool which sets out key signs of MND to help GPs to identify suspected cases and ensure prompt referral.
I recognise the valuable contribution made by carers of people with MND, many of whom spend a significant proportion of their life providing support to family members, friends and neighbours. I agree that carers must receive the right support to help them carry out their caring roles, and a new cross-Government National Carers Strategy is being introduced to look at what more can be done to support existing and future carers.
I was extremely interested to read about the research undertaken by the University of Edinburgh which identified an issue with MND patients' nerve cells, suggesting that this damage could be repaired by improving the energy levels in mitochondria. While I understand that this research is still in early stages, it is a most welcome step forward, and I will certainly follow this closely.
March 2021
Conversion Therapy - Update
Selaine’s response:
I understand the concerns of some people of faith, however I do not agree with those who believe that this law would ‘criminalise Church’. I believe that the Church and religious institutions should be able to preach what they believe in, such as the words of the Bible, however it is my view that this should only be done to those who wish to listen. It is not the intention nor will it be the outcome of the proposed new law to infringe on religious freedom, but instead to protect those in the LGBT community who have already faced much persecution and inhumane treatment.
The Government is aware of the concerns that some constituents have raised regarding religion and faith, and my Ministerial colleagues have said that they will continue to engage with religious organisations and groups to understand how best to support LGBT people of faith. While it is not the Government's place to dictate what is legitimate spiritual guidance, it is the Government’s place to protect all their citizens, some of whom find any act from someone of faith to attempt to change their sexual orientation deeply harmful and traumatic.
March 2021
Conversion Therapy
Selaine's response:
I take this issue very seriously and I know that my colleagues in the Equalities Office remain committed to tackling conversion therapy in the UK. I am absolutely clear that this practice has no place in civilised society, because being lesbian, gay or bisexual is not an illness to be treated or cured.
I am encouraged that this view is shared by the head of the NHS, the Royal College of Psychiatrists, the UK Council for Psychotherapy, the British Association for Counselling and Psychotherapy and the British Medical Association. Each of these bodies have concluded that such therapy is unethical and potentially harmful. The Government Equalities’ Office commissioned a large-scale LGBT survey in 2017. Sadly, 2% of respondents to the national LGBT survey said they had undergone conversion therapy in an attempt to ‘cure’ them of being LGBT. Unfortunately, in this survey, what conversion therapy entailed was not defined, nor were the respondents asked whether or not the conversion therapy referred to in their answer was offered in the UK.
I welcome the firm commitment to preventing these activities from continuing. Led by colleagues in the Government Equalities Office, research is underway to look at the experiences of those subjected to conversion therapy. I have received assurances that Ministers are thoroughly considering all legislative and non-legislative options in order to end conversion therapy practice for good, and will outline their plans in due course.
I am positive about the steps that have been made so far in the UK to achieve LGBT equality, and I am confident that this good work will continue.
March 2021
Medical Freedom Bill
Selaine's response:
While I understand that a range of options are being considered to encourage people to receive the vaccine, the Government does not plan to make the Covid-19 vaccination mandatory.
It is right that we rule out no options at this stage. Conclusions and the outcome of the review will be set out in advance of Step 4 of the Roadmap. As the Prime Minister has said, it may be that there is a role for certification in the future, but for now the emphasis is rightly on our vaccination and testing programmes.
I am satisfied that steps will be taken to appropriately consider the impact of any certification approach and, if necessary, apply relevant safeguards. As such I do not feel a Medical Freedom Bill such as the one proposed by Save Our Rights UK is required.
March 2021
Cancer Treatment and Coronavirus
Selaine's response:
When people start treatment for cancer, their medical team works with them to balance the risks and benefits of treatment before agreeing a plan. As a result of the pandemic, it may be that doctors consider the risks of certain treatments, particularly those that weaken the immune system, to be much greater than normal. They will take into consideration how urgent your treatment is: in some cases, delaying treatment might not make a big difference to the outcome. Patients with cancer visit hospitals regularly, but for those who are particularly vulnerable, this may have been more risky than usual at the height of the pandemic as it may result in exposure to the virus. As a member of the Radiotherapy APPG I did raise concerns about access to cancer treatment during the pandemic directly with the Minister responsible.
The Secretary of State for Health and Social Care announced the restoration of NHS services on 27th April, starting with the most urgent, like cancer care and mental health support. The NHS is open for business, and anyone who needs care and treatment should continue to access it as and when they need it, especially when delays could impose both an immediate and a long term risk to health. I know that continuation of cancer services is absolutely vital in many cases, which is why I welcome that restarting cancer care in a safe manner has been a priority for the NHS and for the Government. I welcome also that, due to covid-19, the 21 cancer alliances in England have established hubs to ensure dedicated cancer care away from hospitals dealing with the virus.
I welcome that the Government has already announced £3 billion funding to support the NHS recovery from Covid-19, to help to ease existing pressures and enable hospitals to carry out extra checks, scans, and other operations or procedures. This will help to ensure that cancer patients are able to access the care that they need as safely and quickly as possible.
Any changes to treatment protocol to ensure patients are treated safely should be carried out in full consultation with patients, to ensure that they fully understand the reasoning behind any changes made in line with guidance from clinical experts. If you have concerns about your own situation, I would strongly encourage you to speak to your medical team to discuss your options.
March 2021
Covid-19 Vaccinations and ME/CFS
Selaine’s response:
The Joint Committee on Vaccination and Immunisation's (JCVI) advised prioritisation list for the initial phase of the Covid-19 vaccination programme was specifically aimed at the prevention of Covid-19 mortality and the protection of health and social care staff and systems. I understand that currently ME/CFS are not listed as specific conditions in the priority list, however those with chronic neurological disease are included in priority group 6.
The JCVI has recently clarified that the examples of clinical risk groups, listed in the Green Book: Immunisations against infectious disease, are not exhaustive, and the advice states that within these groups, clinical judgment should be applied to consider the risk of Covid-19 exacerbating any underlying disease that a patient may have, as well as the risk of serious illness from Covid-19 itself. More information and support, including advice on contacting your GP, can be found on the ME Association website here:
https://meassociation.org.uk/2021/02/latest-covid-19-me-cfs-and-the-jcvi-priority-vaccination-list/
February 2021
Support for Unpaid Carers
Selaine's response:
I recognise the valuable contribution made by carers of all kinds; residential, domiciliary, paid and unpaid; many of whom spend a significant proportion of their life providing support to family members, friends and neighbours. I wholeheartedly believe that carers must receive the right support to help them carry out their caring roles. A tenth of adults in the UK provide unpaid care for a friend or family member, and these people should be supported in the invaluable work that they do.
The Government is committed to supporting the 5.4 million unpaid carers over the coming months. Funding has recently been extended to Carers UK’s support phone line until March 2021 to cover the winter period, and the Department for Health and Social Care has provided free flu vaccines for unpaid carers. In addition, the Department for Education has launched the ‘See, Hear, Respond’ service in partnership with Barnardo’s to support young carers through this challenging time. I am assured that cross-departmental work is ongoing to scope further support options for young carers.
Existing support will remain available including the Carer’s Allowance, as well as through NHS volunteers who can provide support by going shopping or collecting prescriptions. Ministers have committed to regularly updating and bolstering the online guidance for unpaid carers, and I will continue to monitor progress in this area, speaking up for unpaid carers in Parliament.
February 2021
UNICEF: Future at Risk
Selaine's response:
The UNICEF report is correct to note that the pandemic is exerting severe pressure on essential and life-saving health services in many, particularly poorer, countries around the world. This threatens to increase levels of maternal and child mortality, and thus global progress towards achieving Sustainable Development Goal (SDG) 3. Unless decisive action is taken now past progress towards this goal, as with many others, such as education (SDG 4), risks being erased altogether.
I am proud that UNICEF notes that the UK has been at the forefront of global health agendas for decades, with an exceptional aid track record. I am confident that current and future development efforts will honour this reputation. In 2020, for example, the UK pledged a total of £166million dedicated to tackling food insecurity and to provide aid to more than 7 million vulnerable people in some of the world’s most dangerous places.
I appreciate the call for the UK to publish a plan for ending preventable deaths of mothers, new-borns and children. Nevertheless, Ministers have been clear that the UK's approach to this particular issue will be informed by the outcomes of the Integrated Review. Working from first principles in this way is the right approach in my view, thus, it is best to wait until the Review has concluded before the UK commits itself to a detailed course of action on this issue.
I wholeheartedly agree with the recommendation that the UK should aim to lead global efforts to build resilient health systems. The Prime Minister has already set out a five-point plan to strengthen health systems against global health crises, and committed to putting girls' education and empowerment, including reproductive health, on the global agenda as part of our Presidency of the G7 this year.
February 2021
Foster Carer Vaccine
Selaine's response:
The Joint Committee on Vaccination and Immunisation (JCVI) has set out a strategy that prioritises protecting those most at risk of death and serious disease. In line with the recommendations of the JCVI, the vaccine is initially being rolled out to the priority groups including care home residents and staff, people over 80 years old and health and care workers, then to the rest of the population in order of age and risk, including those who are clinically extremely vulnerable and all individuals aged 16-64 years old with underlying health conditions.
Once those most at risk have been protected, Phase 2 of the programme will commence. This may include targeted vaccination of those at high risk of exposure and/or those delivering key public services, such as teachers and foster carers. As with the first phase of the programme, these decisions will be guided by expert advice from the JCVI. My Minsterial colleagues are aware of the case being made for prioritising foster carers.
I am very pleased by the great progress we are making with the vaccination programme. The quicker we get people vaccinated, the quicker we will be able to get back to our normal lives.
February 2021
Alzheimer’s
Selaine's response:
I can only imagine how challenging it must be for families caring for loved ones during this difficult time, particularly those who have needed to take on extra responsibilities. I know that the Government is working closely with system partners, stakeholders, local authorities and the care sector to monitor the impact of Covid-19 on people with dementia and to identify what additional actions may be required to ensure safety, and access to the right support and care.
Research through the National Institute for Health Research was commissioned on how to manage or mitigate the impact of Covid-19 on people with dementia and their carers living in the community. The research has considered the best ways to support people to stay well during the outbreak, including help to manage the psychological and social impacts of social distancing, self-isolation, and lockdown. You can find more information, including summary leaflets, here: http://www.idealproject.org.uk/covid/
I agree that we should do everything we can to offer support to people with long term health conditions, as well as those who support them, throughout this difficult time, and I will certainly continue to monitor this issue closely.
February 2021
Guide Dogs Accessible Vaccinations
Selaine's response:
I can assure you that I take the issue of vaccine take-up incredibly seriously and I welcome the Government's commitment to move the UK's vaccine programme forward with pace. I firmly believe that accessibility is a key priority, and so I welcome that the Department of Health and Social Care has been working to ensure information is provided about the vaccine in audio, Braille, large print, easy read and British Sign Language.
The framework for rolling out the vaccine outlines that providers are responsible for ensuring that their vaccination centres are accessible to all members of their community and they should take steps to improve access and reduce potential inequalities for people eligible to receive vaccinations. Patients booking vaccination appointments can choose a site that meets their accessibility needs and transport requirements and will be informed of the distance of the site from the postcode they have entered.
I am already working with vaccination hubs in North Devon to ensure that everybody can access the vaccine as soon as they are invited to do so.
February 2021
Vaccine – Learning Disability
Selaine's response:
The Joint Committee on Vaccination and Immunisation (JCVI) has carefully considered the prioritisation of those with learning disabilities. Current evidence strongly indicates however that the single greatest risk of mortality from Covid-19 is increasing age and that the risk of a serious health complications increases exponentially with age. When compared to persons without underlying health conditions, the absolute increased risk in those with underlying health conditions is considered generally to be lower than the increased risk in persons over the age of 65. The exception to this being the clinically extremely vulnerable. The JCVI's advice is therefore to offer vaccination to those aged 65 years and over, followed by those in clinical risk groups aged 16 years and over. This includes those with severe and profound learning disabilities.
While the JCVI has given the recommendations on the first phase of prioritisation, The JCVI is still due to come forward with further recommendations of future prioritisation. The JCVI is in the process of considering the next phase of the vaccination programme and they have said that the points raised with them regarding the wider numbers of persons with a learning disability will be taken into account in the relevant discussions and considerations ahead. I will be following the developments closely.
February 2021
FFP3 masks
Selaine's response:
Continuing to ensure our frontline staff are properly protected is of paramount importance to me, and to my colleagues on all sides of the House of Commons.
Over 3 billion items of PPE have been delivered since the start of the outbreak to 58,000 health and care settings. Almost 28 billion items of PPE have been ordered overall from UK based manufacturers and international partners to provide a continuous supply in the coming months and the Government is confident in the stocks and sources of supply of PPE to meet the needs of health and social care over the coming months.
FFP3 face masks are designed for use when carrying out potentially infectious aerosol generating procedures. Risk assessments in the workplace establish when different PPE is appropriate: FFP2 respirators may be more appropriate and deliver the required level of safety for the care a member of staff is delivering and FFP3 masks are not always necessary. The Government has worked with the NHS and with a range of suppliers to ensure that health and care facilities have plenty of PPE of the correct standard.
February 2021
Living with Disabilities during the Pandemic
Selaine's response:
It is troubling that so many people with disabilities feel forgotten during this crisis. As well as addressing this, we must ensure rights are not diminished and look for opportunities to change things for the better for good. Having read Scope's report in detail, I am aware it has been brought to the attention of my colleagues in the Department for Work and Pensions and the Government Equalities Office.
Regarding welfare, the Government acted quickly to suspend all face-to-face assessments for health and disability related benefits while also extending award periods, giving people peace of mind that their benefit payments would continue. By doing this, Ministers are protecting the health of individuals claiming these benefits, many of whom are likely to be at greater risk of severe Coronavirus symptoms due to their pre-existing health conditions.
It is my view that measures in the Coronavirus Act are temporary and proportionate to the threat we face. It is important that they will only be used when strictly necessary and will only be in place for as long as required to respond to the public health emergency. Local authorities are still expected to do as much as they can to comply with their duties to meet needs during this period, and the legislation does not remove the duty of care towards an individual's risk of serious neglect or harm.
February 2021
Vaccine Rollout in North Devon
Selaine's response:
Thousands more doses of the Oxford Astra-Zeneca vaccine have been received from the national supply chain and given to priority groups in Devon this week.
GP practices are prioritising use of the Oxford vaccine for use in older persons’ care homes as it is easier to transport and store.
The NHS has been asked to ensure everyone in care homes has been vaccinated by 24 January and it is our ambition in Devon to achieve this.
The focus now is on ensuring that we deliver to more people in priority cohorts and sooner, especially groups 1 and 2 with all those to group 4 offered a vaccine by the middle of February.
The Joint Committee on Vaccination and Immunisation (JCVI) has advised prioritising delivery of the first vaccine dose as this is highly likely to have a greater public health impact in the short term and reduce the number of preventable deaths from COVID-19.
The COVID-19 Actuaries Response Group has conducted a review into the logic of the UK’s vaccine priority ordering. This document shows the number needed to vaccinate in care homes is 20 vaccinations to prevent one death, compared with other groups in priority 1-4 of between 160 and 600 vaccinations to prevent one death.
I do agree that teachers, police officers and other frontline staff play a critical role and I acknowledge all their hard work throughout this challenging time. The Joint Committee on Vaccination and Immunisation (JCVI) has considered evidence on the risk of exposure and mortality by occupation.
The JCVI noted that occupational prioritisation could form a part of a second phase of the programme, which will target healthy individuals between 16 and 50 years old. As yet, the priority list for the second phase has not been established, however I know that ministers are aware of the importance of vaccinating teachers and teaching staff, the police force and other key worker groups. I look forward to learning more about future priorities.
I understand that people would like to see exact numbers of on how many people have been vaccinated in North Devon. We can extrapolate from what we have seen to say that at least 4000 people have received the vaccine just via the North Devon Leisure Centre Hub.
GPs, pharmacies and mobile vaccination units are being brought into use to enable the programme to reach all parts of North Devon. It is not always appropriate the ask the most vulnerable of our elderly into the Hospital or the North Devon Leisure Centre. The number of people and the number of ways that people are being vaccinated continues to increase each week.
There are 6500 people over the age of 80, so I do believe that we are well on the way, and in line with national projections to start on the over 70s in earnest this week.
I know that the wait is frustrating, we all want to see and hear that our family, friends, loved ones and neighbours have had the vaccine. Every day we get closer to a significant milestone and all the NHS and your local GPs are asking is that we are patient with them and that we wait for their call.
January 18th 2021
NHS frontline workers’ pay
Selaine's response:
I of course share your admiration for the frontline workers who are making immense sacrifices to help those affected by the coronavirus outbreak. Ongoing restrictions continue to present new challenges and our key workers are supporting people across the country.
I fully support the Government's announcement of a pay rise of 2.8 per cent, backdated to April 2020, in line with the recommendations of the independent pay review body for dentists and doctors. This pay rise is an important acknowledgment of the commitment and hard work of staff throughout this difficult time. Staff on the Agenda for Change (AfC) deal are already scheduled to receive pay rises, with the starting salary for a newly qualified nurse increased by more than 12 per cent by the end of the AfC time period, with all nurses receiving pay increases of at least 6.5 per cent; the Government has also introduced a nurses' bursary which provides at least £5,000 of additional support to nursing students. I understand that the NHS Pay Review Body, covering AfC staff, will return to making recommendations for next year's pay awards.
When people voted to leave the EU, they did so in the knowledge that the free movement system imposed by the EU would end. The Home Secretary has been clear that she had a particular responsibility to take back control and end free movement once and for all. I welcome the Government’s commitment to build a fairer single, global immigration system which considers people based on their skills, rather than nationality. The Coronavirus pandemic has proven beyond all doubt the need for an immigration system that will not just allow but actively welcome a range of health professionals to the United Kingdom. I welcome the fact that the Government has ensured that this will be the case. The new Health and Care Visa, creates a new fast-track visa route for eligible health and care professionals.
I am particularly pleased that the Government has taken action to ensure the immigration system does not unduly infringe the ability of the NHS to respond to the Coronavirus outbreak. It is good news that thousands of health professionals and their family dependants will have their visas extended for a year, free of all fees and charges. This comes after a previous announcement offering free visa extensions for health professionals whose visas were due to expire between 31 March 2020 and 1 October 2020. This further action taken by the Government will now extend that offer from 1 October 2020 until 31 March 2021.
The fight against coronavirus is a national effort, and my colleagues and I are committed to giving NHS staff the additional support they need throughout it. The dedication and sense of duty shown by key workers during the outbreak has been exemplary. I am grateful for their work in ensuring that society can continue to function.
January 2021
Coronavirus and IVF
Selaine's response:
I know that this has been an incredibly challenging time for those seeking IVF treatment and I am acutely aware of the time-sensitive nature of IVF.
I understand that the pandemic has been distressing for those undergoing or seeking IVF treatment. I was therefore encouraged that fertility services were among the first to reopen on the 11th May. I was also pleased to see that the Human Fertilisation and Embryology Authority (HFEA) extended the storage limit by two years so that those undergoing fertility treatment during the pandemic could have more time to continue treatment.
Clinical Commissioning Groups should commission fertility services in line with National Institute for Health and Care Excellence (NICE) guidelines which recommend three cycles of IVF. The Secretary of State for Health and Social Care has described the lack of equity as ‘absurd’ and has vowed to end postcode inequalities. Ministers have written to Clinical Commissioning Groups twice in the last eighteen months regarding these unfair variations.
The Secretary of State has said that all fertility patients should be dealt with fairly and not face any additional disadvantage as a result of services being stopped for six weeks. Nevertheless, fertility services remain the prerogative of Clinical Commissioning Groups and I trust that they will make the right decisions. I wold be happy to raise this with our local CCG should any constituents have issues themselves.
November 2020
Publicly-run Test and Trace
Selaine's response:
As part of an unprecedented response to this pandemic, my colleagues in the Department of Health and Social Care have drawn on the expertise and resources of a number of public and private sector partners to support our NHS and social care sector. The Government has been guided by the science throughout, consulting with a range of experts in each field, and has made significant progress in testing capacity and analysis.
Testing and NHS Test and Trace services are being provided through the NHS, and while it is true that providers like Serco and Sitel are working with the public sector to deliver these services, these providers will be held to the highest standards to ensure that the best service possible is delivered. Ministers are confident that 500,000 tests will be able to be processed daily by the end of October and are increasing the number of testing sites by 20 percent, which should enable people to find a test site closer to their homes, as well as increasing testing capacity.
It is a testament to the ingenuity of British businesses that they have been able to adapt existing resources in a time of great need for the country, and I am extremely grateful to all organisations that have offered their services at this time. For an undertaking of this scale, it is inevitable that there needs to be private and public sector cooperation. The public sector alone simply does not have the capacity, and I would highlight that we are carrying out more tests than practically anywhere else in Europe.
October 2020
Flu Jab
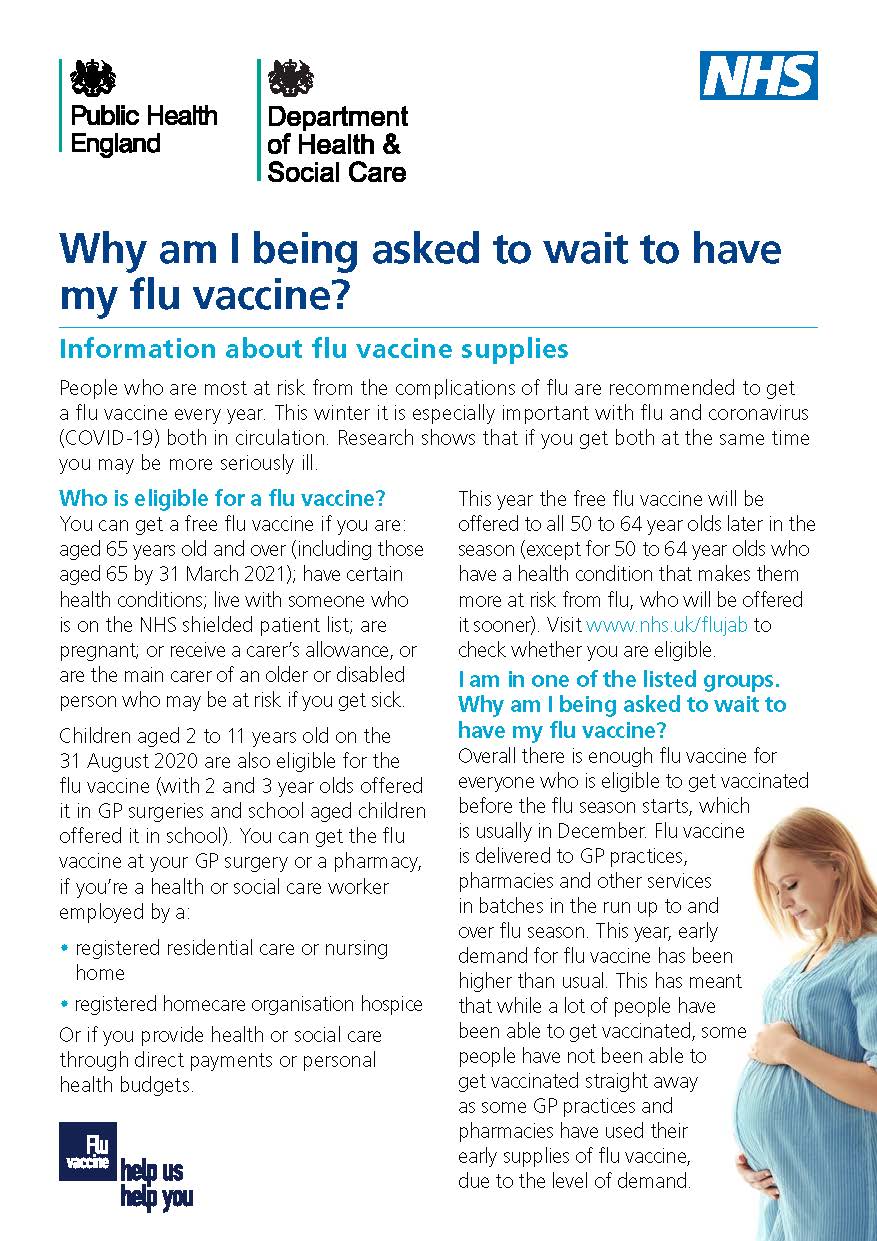
Medicinal Cannabis
Selaine's response:
“There is strong scientific evidence that cannabis can harm people’s mental and physical health, and damage communities. However, recent cases have shown the need to look more closely at the use of cannabis-based medicine in treating patients with very specific conditions in exceptional circumstances. This is why the Government decided it was appropriate to review the scheduling of cannabis.
The decision to reschedule these products means that senior clinicians will be able to prescribe the medicines to patients with an exceptional clinical need. Following short term advice issued in September 2018, the current rescheduling and its appropriateness will be reviewed by November 2020.
Moreover, NHS England has published a review which is aimed at assessing the barriers to prescribing cannabis-based medicinal products where it is safe and clinically appropriate to do so. Steps have been taken to help ensure people with prescriptions for cannabis-based products for medicinal use do not have their treatment delayed or interrupted, by altering import restrictions. This is a welcome step towards improving the supply of cannabis-based medicinal products.
The National Institute for Health and Care Excellence (NICE) has also developed updated clinical guidance on prescribing cannabis-based products for medicinal use, including for the management of chronic pain. It is crucial that this country keeps in step with the latest scientific evidence, so that patients and their families have access to the most appropriate course of medical treatment. My Ministerial colleagues have also been clear that given the nature of the medicine, it should only be prescribed be specialist doctors and on a case-by-case basis. I believe these controls are necessary to develop clinical expertise and an evidence base for this treatment’s effectiveness.”
October 2020
Coronavirus Act 2020 (Review of Temporary Provisions) (Motion)
Selaine's response:
“On the subject of scrutiny, Mr Speaker voiced his concerns today in the Chamber, and I am one of those that will be unable to speak in the debate today, being 56 on the call list. No amendments were selected by Mr Speaker because of the binary nature of this legislation and you can see his statement below. I would also like constituents to be aware that many of the restrictions that have been imposed have been implemented under the Public Health (Control of Disease) Act 1984, not the Coronavirus Act 2020.
The Government has listened to the concerns of backbenchers this week with regards to increased scrutiny of emergency measures and this has been detailed in the Chamber this afternoon by Health Secretary, Matt Hancock. All measures affecting the whole of England or the whole of the United Kingdom will be subject to a vote in the House of Commons wherever possible. The Secretary of State has also detailed that only those measures in the Act which are strictly necessary will be renewed, and I know a number of constituents were concerned about some of the powers given to the Government. Some of the powers relating to the Mental Health Act 1983 and sectioning will not be renewed, for example.
Therefore at this time, to ensure clarity through this unprecedented period I, along with Sir Graham Brady, will be supporting the Government to extend the emergency coronavirus legislation this afternoon."
September 2020
Click here for Mr Speaker's statement on the matter: https://parliamentlive.tv/event/index/30624341-5d7c-4599-ad0c-3dc106647…
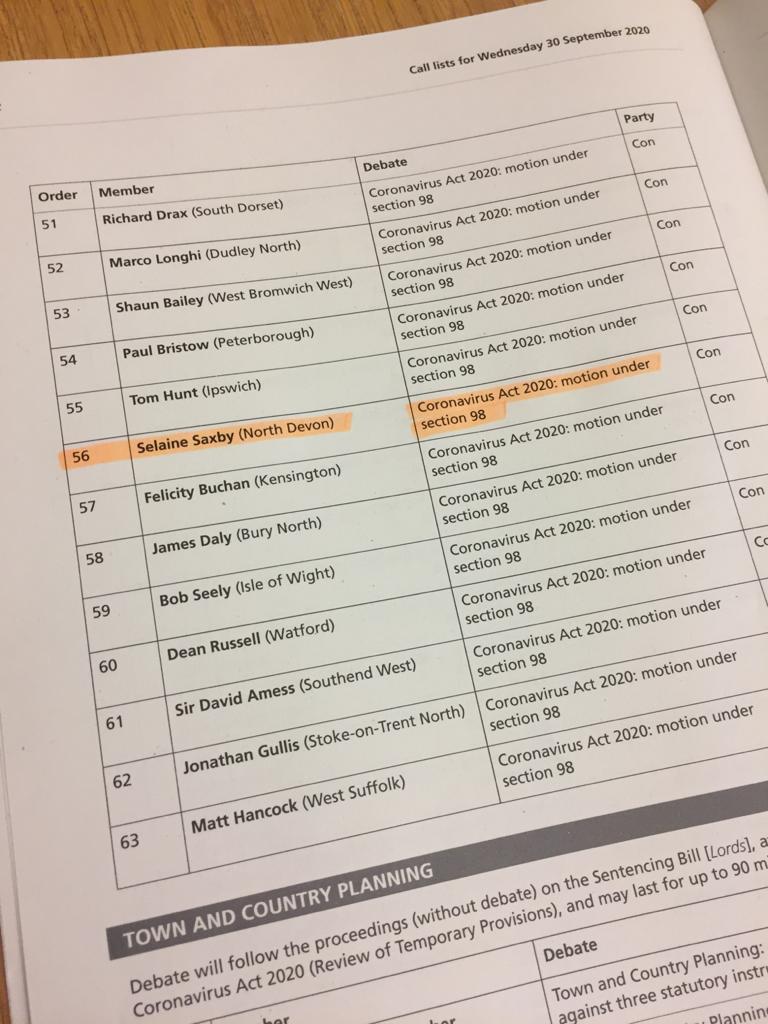
Coronavirus and Mental Health in Schools
Selaine's response:
“I share your concern about the impact the coronavirus outbreak will have had on children and young people's mental health. In particular, being separated from their peers for such a long period of time poses a real risk to young people's mental health, as well as hampering their social development.
As such I am very pleased that schools and colleges have reopened. Recognising that some children and staff will need support as they make the return to education, it is very welcome that action is being taken to improve mental health support, with the Wellbeing for Education Return programme launching to improve the wellbeing of pupils and staff in schools and colleges. The £8 million programme will support staff working in schools and colleges to respond to the additional pressures some children and young people may be feeling as a direct result of the pandemic, as well as to any emotional response their staff may still be experiencing from bereavement, stress, trauma or anxiety over the past months. The programme has been created with input from heath partners, mental health experts, local authorities, and schools and colleges. The Department is also inviting educational psychologists to express an interest through their local authorities in providing temporary support for children and young people returning to educational settings in September 2020.
This action comes on top of the existing commitment to invest at least £2.3 billion of extra funding a year into mental health services by 2023-24 through the NHS Long Term Plan. This funding underpins the aim for an additional 345,000 children and young people to be able to access support through NHS-funded services or school and college based mental health support teams.
I welcome the action outlined above, and I agree with you that it is vital mental health support is properly funded. As such I will be pressing ministerial colleagues to ensure these services are considered in this year's Spending Review.”
September 2020
Arthritis and Covid-19
Selaine's response:
I know that arthritis can be an incredibly painful and debilitating condition, and we do need to ensure that people with arthritis are getting the treatment they need as the NHS begins to return to normal. I would like to set out some of the steps the Government is taking to make sure that happens.
The NHS is being provided with an additional £33.9 billion by 2023/24; this is the largest, longest funding settlement in the history of the NHS. This landmark investment to help secure the long term future of our NHS is extremely welcome, and I hope you agree it demonstrates the Government’s commitment to properly funding our NHS and public services: health is the Government's top priority.
Alongside this, the NHS was asked to undertake a clinical review of standards relating to waiting times. This must be clinically led to enable best, and safest, delivery of care for patients. I understand that NHS England has now prepared proposals, covering waiting times across the service, including elective procedures, mental health, cancer, and A&E. I understand that the recommendations following this review have been deferred as part of the NHS response to the Covid-19 pandemic, which is understandable. I will be sure to study these in due course.
I know that, while it has been important to postpone some NHS activities to protect individuals and enable resources to be used as efficiently as possible, my colleagues in the Department of Health and Social Care, as well as NHS Staff, are determined to restart elective procedures as soon as it is safe to do so. The exact pace of this restoration is determined by local circumstances, according to local need and demand, and according to the number of coronavirus cases being dealt with by the hospital. I have been in regular contact with the Northern Devon Healthcare Trust about this and other issues.
August 2020
Fix Dementia Care
Selaine's response:
I believe we must all receive dignified care in old age. With an ageing population, this is one of the biggest challenges our country faces. I support the Government’s commitment to making sure that the most vulnerable in society gain the support they need. Whilst it is important to note that more than 4 of every 5 people in care receive care from good and outstanding organisations, it is clear that more needs to be done to tackle this serious challenge – crucially by securing a long term funding solution. I am delighted that the Prime Minister has spoken of his determination to tackle this, stating in his first speech as Prime Minister that “we will fix the crisis in social care once and for all with a clear plan we have prepared, to give every older person the dignity and security they deserve”.
The Government is currently producing a Social Care Green Paper, which will consider a range of proposals to improve social care, as well as funding options to ensure our social care system is able to meet the needs of our ageing society and is placed on a sustainable footing for the long term. Since 2015 local authorities have had greater flexibility over the use of the council tax social care precept, so they can choose to raise extra money, as well as retain savings from the New Homes Bonus, totalling £240 million.
In the Spending Round in September, an extra £1.5 billion was made available to councils for adult social care services. This funding should be viewed as a significant down payment as we move towards a long term funding solution.
Money alone will not fix the problem and reform is needed to encourage high standards across the whole country. It is vital for us to consider ways of better joining up health and care services, and I am encouraged by the use of the Better Care Fund to assist local government and the NHS with the implementation of integrated health and care services.
July 2020
Shielding and Blood Cancer
Selaine's response:
It is crucial that those at most risk in our society are protected in order to safeguard their own health and prevent the NHS from being overwhelmed. I am also greatly saddened to hear of financial difficulties at this time. No one following Government instruction, should be penalised for their efforts.
I do not wish to see anyone put at any risk as the lockdown is eased. I have been reassured by colleagues in Government that they are following the best medical advice for getting people back to work. I strongly encourage employers who employ people with blood cancers to utilise the Coronavirus Job Retention Scheme (CJRS) for as long as possible until the safety of such employees can be guaranteed. As I am sure you are aware, the CJRS has been extended until October and it should be used where necessary. I would also like to take this opportunity to remind employers that they have a legal responsibility to ensure their employees and other people on the premises are protected.
July 2020
Carer’s Week
Selaine's response:
As a member of the Department for Work and Pensions Select Committee, I am particularly conscious of the invaluable contribution made by carers, and how our society could not function without their work. I recognise the vital contribution made by the multitude of different carers: residential, domiciliary, paid, unpaid. Many carers spend a significant proportion of their life providing support to family members, friends and neighbours. I agree completely that carers must receive the right support to help them carry out their caring roles. A tenth of adults in the UK provide unpaid care for a friend or family member, and these people should be supported in the invaluable work they do.
That is why a cross-Government National Carers Strategy was introduced to look at what more can be done to support existing and future carers. After a lengthy consultation with carers, the Government announced a two-year programme of support. This includes support for young carers, effective action to help carers balancing their caring and employment responsibilities, and ensuring that health and social care services are responsive to their needs.
The Government is continuing to support the implementation of improved rights for carers, enshrined in the Care Act 2014. I welcome the fact that benefits to support vulnerable and disabled people, including Carer’s Allowance, are exempt from the freeze on working-age benefits. I am also glad to note that the Department of Health and Social Care will continue to lead a programme of targeted work to support carers.
This year, Carers' Week has fallen during the coronavirus pandemic, a time which has highlighted the invaluable work carried out by carers, both paid and unpaid. I am pleased the Government has fulfilled its commitment to offer tests to all adult care homes for over-65s for their residents and staff. At the beginning of June, a new Social Care Sector Covid-19 Support Taskforce, chaired by David Pearson, was also announced. It will work to tackle and control the transmission of the virus in social care. I will continue to work with the Government throughout this difficult time in particular to ensure that carers are able to access the support that they need.
June 2020
NHS Testing (Opposition Day debate - 24/06/20)
Selaine's response:
I am aware that a number of people have raised the issue of the Opposition Day Motion yesterday, which proposed a weekly testing programme for NHS and social care staff. To be clear, I am not against regular testing of NHS staff. However, the Opposition Day Motion is not what the Chief Medical Officer has recommended, and the Government is following his advice.
Professor Chris Whitty has recommended a fortnightly testing programme which can be more frequent if the local or national epidemiological conditions demand, e.g. if there is a local outbreak or if national levels of transmission rise. NHS England and NHS Improvement have written to NHS Trusts across the country to ensure this is implemented. Testing is continuing to be prioritised for NHS staff who have symptoms to ensure that they can continue to work if they do not have Covid-19.
I was present for this debate and I spoke about the hard work of all those at North Devon District Hospital, in our social care sector, and at Public Health Devon. I listened carefully to all the contributions made during the debate and I was not entirely sure that the Shadow Secretary of State for Health was clear about the content of his motion. The motion asked for a weekly testing programme, whilst in his speech he only asked for weekly testing ‘if necessary’. Weekly testing ‘if necessary’ is completely consistent with the Government’s position.
It is also worth highlighting the fact that the Government’s amendment to the Opposition Day Motion passed without a vote, meaning the opposition did not oppose it.
June 2020
Abortion (Northern Ireland) (No. 2) Regulations 2020
Selaine's response:
I voted in favour of the above legislation on 17th June, and I want to explain why I made that decision to those constituents who contacted me.
This vote was about standardising the legislation on abortion across the whole of the United Kingdom. I agree that the Northern Ireland Assembly should be allowed to have its say, but the origin of the duty for the UK Government to legislate on this issue stems from the Assembly not having sat for several years. Legislation was therefore passed in July of last year which aimed to standardise abortion law but which stated that if the Assembly were restored by a set date, the law would not change. The Assembly failed to come to an agreement which led to its restoration, and so the Government are under a legal obligation to act.
In fulfilling its obligation, the Government has sought to mirror provisions under the Abortion Act 1967, and a consultation was held on the proposed framework. Whilst the Northern Ireland Assembly did vote against this change, it did so during a plenary session and so the vote had no bearing on the legislation. The Government’s legal duty to legislate therefore remains. However, the Assembly is free to amend the regulations so long as those amendments are compliant with the 1979 CEDAW Treaty.
June 2020
Abortion (Cleft Lip, Cleft Palate, and Clubfoot) Bill
Selaine's response:
The approach to abortion in Great Britain is set out in the Abortion Act 1967, which states that two doctors must certify that, in their opinion, a request for an abortion meets at least one and the same ground laid out in the Act. These grounds include “risk to the life of the pregnant woman”, and “substantial risk that if the child were born it would suffer from such physical or mental abnormalities as to be seriously handicapped”.
There is guidance for doctors on how to comply with the Act has been issued, which stipulates that registered medical practitioners should be able to show how they have considered the particular facts and circumstances of a case when forming their opinion. Full details can be found online at www.gov.uk/government/publications/guidance-for-doctors-on-compliance-with-the-abortion-act. Not every pregnancy goes to plan and foetal abnormalities of varying degree of severity occur. Women need support and information to reach an informed decision about how to proceed. Health professionals must adopt a supportive and non-judgemental approach regardless of whether the decision is to terminate or continue the pregnancy.
Before making a decision about my position on this Bill, I am waiting to see the full text of the proposed legislation. I will then consider whether it is something I can support.
June 2020
Prison Safety and Coronavirus (plus Julian Assange)
Selaine's response:
I welcome the collaborative approach taken by Public Health England (PHE) and Her Majesty's Prison and Probation Service (HMPPS). This is essential to ensure the implementation of measures to keep prisoners and prison staff safe, protect the NHS and enable the continued operation of the prison estate.
Early data emerging indicates that explosive outbreaks of Coronavirus are not being seen across the prison estate and PHE modelling suggests that the measures introduced are demonstrating that jails are successfully limiting deaths and the transmission of the virus within the estate. I understand that this has been driven by a combination of increased social distancing, reduced transfers of prisoners between prisons and acting within individual prisons to reduce infection. This has reduced the Reproduction Number (or R) to 1 or below. However, until a vaccine or effective treatment has been found, the risk of large outbreaks remains. Ministers will of course continue to review and closely monitor the prison estate.
I understand many constituents have concerns regarding court cases as the outbreak continues. Courts provide a vital public service and justice must be delivered wherever possible. I welcome the fact that Her Majesty's Courts and Tribunals Service have increased the capacity for telephone and video hearings to allow for remote hearings where appropriate. The decision to hold a hearing by telephone or video is for the judge, panel or magistrate, taking into account the needs of the parties, including their ability to access and use the right technology.
Some constituents have contacted me about this topic and how it relates to the safety of Julian Assange. It would not be appropriate for me to comment on an individual case, but the above measures are in place to ensure the safety of all in the UK’s prisons.
May 2020
Trade Bill NHS Campaign
Selaine's response:
The Trade Bill is an important piece of legislation which has a number of functions.
First, the UK has been working to reach continuity agreements with countries who we currently trade with through EU trade deals. The Trade Bill will enable these continuity agreements to be embedded into UK law so that the agreements can be fully implemented. In addition, in leaving the EU, the UK will be acceding to the World Trade Organisation’s Agreement on Government Procurement (GPA) in its own right. The Bill’s provisions will make sure the UK can implement procurement obligations under the Agreement, ensuring continued access to £1.3 trillion per year of global procurement opportunities for UK businesses. As an independent member of the GPA, the UK will be free to decide what procurement is covered under the agreement. Ministers have made clear that the UK’s GPA coverage does not and will not apply to the procurement of UK health services.
The Bill will also facilitate the creation of a new Trade Remedies Authority (TRA), to deliver a new UK trade remedies framework, which among other things will include protections for UK businesses from unfair trade practices or unforeseen import surges.
It is important to make clear that the Trade Bill is a continuity Bill, and its functions are largely distinct from the Government’s future trade agreements programme. Indeed, the Bill cannot be used to implement new free trade agreements with countries such as the US. The Bill simply enables the 40 free trade agreements that the EU had signed with third countries before the UK exited to be transitioned. Separate work on the future trade agreements programme is of course also pressing ahead, with negotiations already underway with the US, and soon to begin with Japan.
With specific regard to a UK-US free trade agreement (FTA), I believe that as our economy recovers from the challenges posed by COVID-19, we need to be negotiating enhanced trade ties rather than putting up barriers. I am reassured by my Ministerial colleagues’ commitment not to compromise the UK’s high animal welfare, environmental, food safety and food import standards in any future FTA, including one with the US. Ministers do not want to compromise the UK’s domestic welfare production standards either. I want to be clear that the NHS will also be protected in any future trade agreement, including one with the US. The price the NHS pays for drugs will not be on the table, and nor will the services the NHS provides.
It is important to make the distinction between the Trade Bill and the Government’s future trade agreements programme. The process of negotiating future trade deals is not primarily a matter for the Trade Bill. However, I want to reassure you that there will be opportunities for both the public and Parliament to consider, contribute to and scrutinise negotiations for future free trade agreements. Public consultations will run ahead of all negotiations, and a number have already taken place, including for negotiations with the US, Japan, Australia and New Zealand. Ministers have also committed to provide Parliamentarians, UK citizens and businesses with access to the information they need on trade negotiations.
May 2020
Children’s Services
Selaine's response:
I agree that our children’s services need proper financial support. I am pleased that in the 2019 Spending Review the then Chancellor made an additional £1 billion available to help local authorities meet rising demand for both children and adult social care. I also welcome that £84 million has been allocated over a period of five years to assist up to 20 local authorities to enhance their social care services, ensuring that they are able to engage more effectively with those who need support the most.
That said, I recognise that there needs to be a longer-term solution to ensure sustainable funding for children’s social services, and to ensure that funding is fairly distributed across the country. I welcome the conclusion of the review into the support available for children in need, which looked at what makes a difference to the educational outcomes of children in need and what works in practice to improve those outcomes. I am assured that the findings of the review will be acted on to inform and improve policy.
I hope this has provided a measure of reassurance. I will continue to closely monitor funding levels for children’s social services.
May 2020
Northern Ireland Abortion
Selaine's response:
I appreciate the strength of feeling about the issue of abortion and I welcome the balanced and sensitive approach the Government has taken. As the Northern Ireland Executive was not restored by 21 October 2019, it remained the UK Government’s legal obligation under section 9 of the Northern Ireland (Executive Formation etc) Act 2019 to bring forward the framework to provide lawful access to abortion services in Northern Ireland by 31 March 2020.
Following a consultation, the Government has now brought forward the new framework. I believe it delivers abortion reform for Northern Ireland consistent with the United Nations Committee on the Elimination of Discrimination Against Women Report recommendations.
The new framework does provide clarity and certainty for medical professionals and also ensures the health and safety of women and girls in Northern Ireland. I have attended a briefing from the Northern Ireland Minister who has explained why this legislation is worded differently to the legislation in the rest of the UK, which is now over 50 years old. The Minister has also met with the Northern Ireland Health Minister as the implementation and commissioning of abortion services will be a matter for the NI Health and Social Care Board to take forward. Further information about the reforms can be found on the Northern Ireland Office website.
May 2020
Welfare of Care Workers
Selaine's response:
I want to first express my gratitude to care workers for the incredible way in which they are doing a very difficult job. We all owe keyworkers a debt of gratitude and I agree that we must recognise their efforts appropriately.
Once we have beaten Coronavirus, we will all have to reassess the way we do things and ensure that the social care sector is put on a stable footing for the foreseeable future. The Government is committed to cross-party talks on the future of social care, and these talks will be wide-ranging and include issues such as pay.
In the meantime, I have been working to ensure that care homes have the Personal Protective Equipment (PPE) they need. The distribution of PPE is a challenge of huge proportions and any care home having difficulties can contact me and I will do my best to resolve them. The Government is doing everything it can and I am in constant contact with Ministers to ensure that PPE gets where it needs to be. Devon has sufficient supplies of PPE and I am working to make sure it stays that way. There is a new national PPE helpline available to those who need PPE here: 0191 283 6543 or email supplydisruptionservice@nhsbsa.nhs.uk . Anyone having difficulties can also use this facility set up by a local company, Applegate: https://www.applegate.co.uk/covid19
If you know of somewhere still struggling to get PPE, please do email me and I will escalate it and ensure that this is delivered as soon as possible. The Government is doing everything it can to get supplies to the right places but it is an enormous challenge.
April 2020
Young People’s Mental Health
Selaine's response:
It is incredibly important to protect and support the health of children and young people in our society; approximately 10 per cent of 5 to 16 year olds have a clinically diagnosable mental health problem.
Between 2015 and 2020, an additional £1.4 billion has been invested to transform children and young people’s mental health. This aims to help an additional 70,000 children and young people to access NHS specialist services a year by 2020/21. Schools and colleges will also be incentivised to train designated leaders for their pupils’ mental health, and introduce new mental health teams, both of which will ease pressure on NHS mental health services.
In addition, the NHS is on track to deliver new waiting time standards for eating disorder services by 2020/21. Four fifths of children and young people with an eating disorder now receive treatment within one week in urgent cases and four weeks in non-urgent cases. Extra investment will enable maintained delivery of the 95 per cent standard beyond 2020/21.
I know in North Devon, the waiting lists for mental health support are often too long, and I have been working with the Department of Health and our local NHS to try and improve the situation. I will put the event on 30th March in my diary and make every effort to attend.
March 2020
NHS Waiting Times
Selaine's response:
The NHS was asked to undertake a clinical review of standards relating to waiting times. I think it is important that any decision to alter the targets for waiting times in A&E must be NHS-led. Accordingly, the NHS has undertaken a clinical review of standards relating to waiting times, and has now prepared proposals covering waiting times across the whole of the health service. This includes waiting times for joint replacement waiting times, something many constituents have contacted me about.
The Government will now carefully consider the proposals before taking any next steps, and in the meantime will continue to hold the NHS to account on its existing standards.
In the meantime, the Government is investing to reduce existing waiting times which I know are too long in many different areas of the NHS. This investment includes an extra 50,000 nurses and 6,000 GPs, which should go a long way to improving the situation. As far as North Devon is concerned, we have always had recruitment issues due to our relative isolation, and I am working with our NHS Trust to find solutions.
March 2020
Protests Outside Abortion Clinics
Selaine's response:
This country has a proud history of allowing free speech but the right to peaceful protest does not extend to harassment or threatening behaviour. The law already provides protection against harassment and intimidation, and the police have a range of powers to manage protests. Like all members of the public, protesters are subject to the law and suspected criminal offences must be robustly investigated and dealt with by the police.
Following concerns about the tactics of protestors outside some abortion clinics, a review was instigated by Government in 2018. This review revealed that anti-abortion demonstrations take place outside a minority of facilities. In 2017 for example, 363 hospitals and clinics in England and Wales carried out abortions. Of those, 36 hospitals and clinics experienced anti-abortion demonstrations. With this in mind, the Government decided that introducing national buffer zones would not be an appropriate response given the experiences of the majority of hospitals and clinics.
That said, while I do not want to see peaceful protest curbed, it is completely unacceptable that anyone should feel harassed or intimidated simply for exercising their legal right to healthcare advice and treatment. The decision to have an abortion is already an incredibly personal one, without women being further pressured by aggressive protesters.
March 2020
NHS & Trade Deals
Selaine's response:
Under this Government, the NHS will always remain free at the point of use and in public ownership. I would not support anything which meant the privatisation of the NHS or additional costs on healthcare for those who need it.
Free trade is a driver of economic growth which can raise incomes, create jobs, and lift people out of poverty, which is why I am glad that outside of the EU the UK will be able to strike new trade agreements with countries across the globe. That said, more trade should not come at the expense of the high levels of quality and protection enjoyed in our country.
The UK will continue to ensure that the NHS is protected in all trade agreements it is party to. Outside of the EU, rigorous protections for our NHS will be maintained and included in any future trade agreement which the UK negotiates.
February 2020
Abortion in Northern Ireland
Selaine's response:
I am pleased that the Government recognises the sensitivity of this issue and the range of views expressed by people on all sides of the debate. It is a highly sensitive issue, regardless of where your view lies and one where it is important that the matter is considered with due care and sensitivity.
The Government is working towards the laying of regulations for a new legal framework for the provision of abortion services in Northern Ireland, as required by the 2019 Act. The new framework will be in force by 31 March 2020.
To help inform the shape of the legislation that is introduced, a consultation was held. This has now closed, and the Government is due to publish its response shortly. I very much welcome the Government’s commitment to ensure that the health and safety of women and girls, and clarity and certainty for the medical profession, are at the forefront of their considerations.
February 2020
Eye Care
Selaine’s response:
To ensure early diagnosis of eye disease, it is important that people are encouraged to get their eyes tested on a regular basis. Clinical advice states that most people should get their eyes tested every two years. Free NHS eye tests are available for those diagnosed with diabetes or glaucoma and those aged 60 or over. This helps to encourage people at particular risk of developing eye disease to have their condition checked regularly. The latest figures show around a 10% increase in the number of eye tests since 2010 so some progress is being made.
I also welcome the broad range of support available for those diagnosed with visual impairments. Many hospitals have Eye Clinic Liaison Officers, or similar early intervention support staff, who provide the practical support which patients need following their diagnosis, including advice on how to deal with their sight loss and maintain their independence.
I will liaise with the Health Secretary about this issue to make sure that North Devon is able to deliver the service that people with sight problems deserve and expect.
January 2020
Immigration Health Surcharge
Selaine’s response:
I believe that overseas visitors should be able to access our NHS as long as they make a fair contribution, just as the British taxpayer does. The NHS is a national - not an international - health service and I commend the Government’s determination to stamp out misuse of the system to ensure it remains free at the point of need in this country.
After a review of the evidence, the annual surcharge will now cost £400 per annum, with a discounted rate of £300pa for students (and their dependants) and Youth Mobility Scheme applicants. The proposed amount is still below full average cost recovery level, which is calculated as £470. The UK must protect its reputation as a great place to live, work and study, and increasing the IHS still offers access to far more comprehensive services at a lower cost than some of our main competitor countries.
The IHS applies to those living in the UK temporarily. Those with indefinite leave to remain and vulnerable groups, including asylum seekers and refugees, are exempt from the charge. It is only right that people who come to the UK for more than six months should contribute to the running of the NHS.
People for whom the IHS applies work in a broad range of jobs fulfilling important jobs in the public and private sectors, jobs that keep the country running. I believe that the IHS should be applied equally, to all non-EEA residents who are in the country temporarily. All residents will benefit from the £220 million funding for the NHS that this fund will provide. The answer is not therefore to exempt nurses from the charge, but to increase their pay; and this is happening.
This charge was brought in to ensure that temporary users of the NHS from outside the EEA are making a fair contribution to the functioning of our national asset, regardless of their employment status. Although some temporary migrants will be paying tax and National Insurance contributions, they will not have made the same financial contribution to the NHS which most UK nationals and permanent residents have made, or will make, over the course of their working lives. It is therefore fair to require them to make an up-front and proportionate contribution to the NHS.
January 2020




